Ecstasy can reduce fears and stress in PTSD patients. Here's how.

When ecstasy hits, it unleashes a rush of euphoria and abundant compassion in users. That's precisely why the drug could be an effective treatment for people suffering from post-traumatic stress disorder (PTSD), early studies show.
A large-scale clinical trial is set to move forward next year to test the therapeutic benefits of MDMA—a.k.a. ecstasy, or molly—in survivors of war combat, sexual assault, violent crimes and other traumatic experiences.
SEE ALSO: New artificial intelligence technique could erase fear from your brain
This week, the Food and Drug Administration said researchers could move ahead with the trial after a series of smaller trials proved successful. The bigger Phase 3 trial could pave the way for the agency to approve ecstasy as a legal drug within a few years.
"It changed my life," C.J. Hardin, a U.S. Army veteran who served three tours in Iraq and Afghanistan, told the New York Times.
"It allowed me to see my trauma without fear or hesitation and finally process things and move forward," he said.
Promising results push FDA to green light broad trials for Ecstasy as treatment for PTSD https://t.co/yS1mNo4eHY
— David Philipps (@David_Philipps) November 29, 2016
Hardin participated in an earlier clinical trial in South Carolina that combined weeks of psychotherapy with limited doses of MDMA, administered under a psychiatrist's guidance. The Phase 3 trial could follow a similar approach, and include hundreds more patients.
Like so many street drugs, ecstasy use comes with (and is also known for) a wide array of health risks, like high fevers, liver failure, cardiac arrest or brain damage. But the drug remains popular among recreational users for its "prosocial" effects—the increased sensations of friendliness, affection and trust.
Studies of MDMA's effects on the brain show the drug triggers the release of a hormone called oxytocin, thought to bring about those prosocial feelings. Ecstasy may also tamp down feelings like fear or threat, by weakening activity in the brain's amygdala region.
Two 2014 studies found that MDMA reduced subjects' abilities to perceive negative emotional states in other people. Not only that, but the drug also made participants less bothered by social rejection.
Like MDMA, PTSD also significantly alters brain activity—but in a completely different way.
Traumatic stress can cause increased activity in the fear-stoking amygdala region, studies show. It also interferes with neurochemical systems that moderate stress and affect memory functions.
By combining MDMA with therapy, patients can quiet their disabling fears and explore the root of their trauma in a more productive way, said Brad Burge, communications director for the Multidisciplinary Association for Psychedelic Studies, a small nonprofit funding MDMA clinical trials.
"When people are processing extremely difficult or fearful emotions, as is the case with PTSD, it can be very helpful in allowing people to clearly describe what they're experiencing," he told Mashable by phone from Santa Cruz, California.
Hardin, the U.S. veteran, said ecstasy helped him climb out of a world marked by sleepless nights and dreams of explosions and death. "The MDMA sessions showed me a light I could move toward," he told the Times from his home in Charleston, South Carolina.
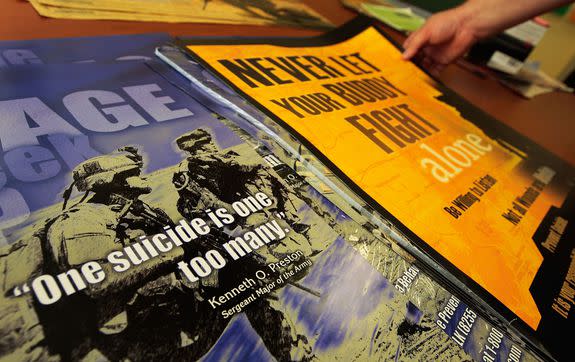
Image: Chris Hondros/Getty Images
Ann and Michael Mithoefer, a wife-and-husband team leading clinical trials in South Carolina, said they found a combination of non-drug therapy sessions and drug-assisted sessions together reduced a range of negative symptoms in their patients.
In one trial, the patients reported a 56 percent drop in the severity of symptoms like general anxiety, depression and nightmares. At the end of the study, two-thirds of patients no longer met the criteria for having PTSD, according to the Mithoefers' research published in the Journal of Psychopharmacology.
Follow-up exams with patients found the improvements lasted over more than a year after therapy.
The trail was one of six Phase 2 studies backed by the Multidisciplinary Association for Psychedelic Studies. Burge said that among the 106 total participants, 66 percent no longer had PTSD by the end of the trial.

Image:
The association as of now is the only U.S. organization driving clinical research in MDMA for therapeutic use in PTSD.
The drug first emerged from the labs of German drug manufacturer Merck in the 1910s. In the following decades, researchers—included the U.S. Army in the 1950s—explored the synthetic drug's potential uses in psychotherapy and psychiatry.
But when ecstasy became a popular club drug in the 1980s and 90s, governments worldwide cracked down. U.S. regulators in 1985 placed the pill on a list of prohibited substances that included heroin and LSD. The association was created that same year.
Burge said the organization needs to raise at least $20 million to support three to four years of Phase 3 trials. A chunk of that money will go toward paying a drug manufacturer to make pharmaceutical-grade MDMA for the research.
He said he expects the FDA to formally green-light the Phase 3 trial in early 2017, and potentially approve the drug for prescription use by 2021.
"We see a very clear path ahead," Burge said. "More people are realizing that we need better approaches to the treatment of PTSD. That's contributed to more [societal] openness toward this research."
Medical experts who spoke with the Times said they were hopeful out the upcoming clinical trials but remained wary of the potential for drug abuse. After all, opioid painkillers like OxyContin are prescription drugs. And the U.S. is now suffering an epidemic of opioid addiction.
"It's a feel-good drug, and we know people are prone to abuse it," Dr. Charles R. Marmar, the head of psychiatry at New York University’s Langone School of Medicine, told the newspaper. Marmar is a leading PTSD researcher and was not involved in the study.
And of course, prolonged use of ecstasy might harm the brain, several studies have shown.
A 2011 study found that long-term users risk damaging their brain structure and developing significant memory problems. Another study in 2013 found long-term ecstasy use may alter brain activation in regions that affect verbal memory.
Still, Marmar said it "will be of great use" if the clinical studies show positive results.
"PTSD can be very hard to treat," he told the Times. "Our best therapies right now don't help 30 to 40 percent of people. So we need more options."

