3 months into Missouri's Medicaid renewal, paperwork is costing many their health care
Springfield resident Eric Honeycutt thought that he and his son had lost their coverage through MO HealthNet, Missouri's Medicaid program.
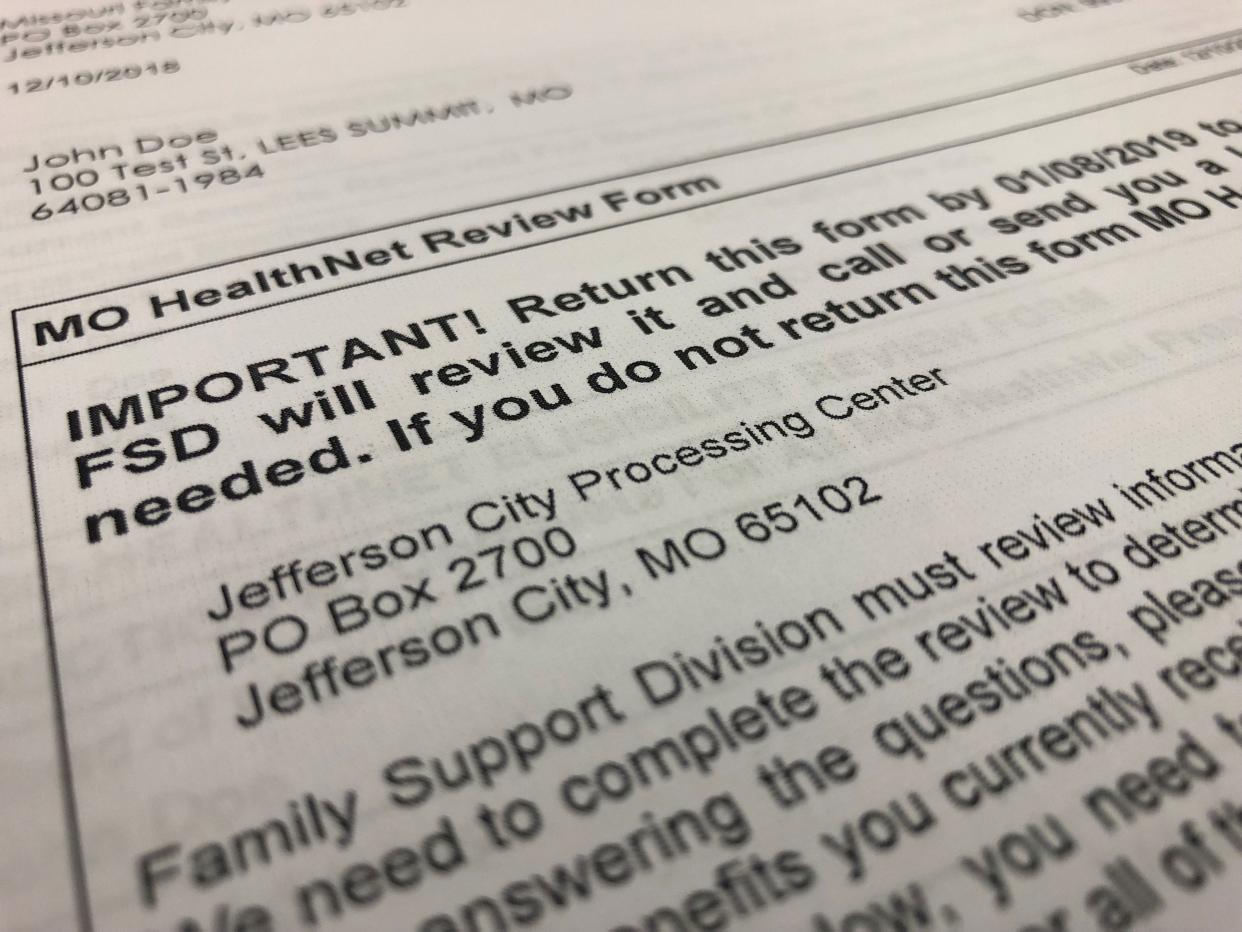
Near the end of September, Honeycutt said he received a letter informing him that his eligibility was denied because he hadn't turned in required paperwork. But he said he sent in the paperwork well before deadline.
Around the same time, his son's counselor called to tell them the medical billers found his son's Medicaid was also cancelled and that his son "wouldn’t be able to get his therapy unless we did self-pay, which is too expensive for us," Honeycutt said.
However, Honeycutt said when he called DSS, he was told something different.
"I called in and found out that my coverage was still active but was pending the renewal process because there’s something like one million people who need to be re-certified," Honeycutt said.
Honeycutt's son didn't lose his coverage, but in August nearly 13,000 Missouri children were deemed ineligible for health care benefits. More than 75% of those were removed for procedural reasons, meaning that there were issues with the paperwork and not necessarily due to the child being ineligible.
Verification of Medicaid eligibility reveals that over a three-month period almost 40,000 kids lost health care coverage.
Renewal, notifications are a work in progress
Some states have experienced a glitch in the verification process that calculates household eligibility rather than individual eligibility.
This led to over 12,000 people being erroneously deemed ineligible in Kansas. Missouri, however, says that it has not experienced this issue.
Department of Social Services spokesperson Caitlin Whaley said that the number of children being disenrolled is in line with the number of children who receive Medicaid. Kids make up about half of all enrollees.
“The number that are being disenrolled is roughly proportional to the amount of kids that are on Medicaid relative to the overall population,” Whaley said.
This is Honeycutt's first time renewing coverage. He's concerned about the process, since he has heard that many people are having experiences similar to his own.
"There’s a ton of people who are getting the same notices that their coverage is declined and not active. Then when they go through the time to call back into the Medicaid office, everyone is finding out no, it’s still active, it’s just going through the process of being re-certified," Honeycutt said. "The only thing you can do is call in and hope the person that you talk to knows what’s going on."
Whaley said there is no way of knowing the reason a denial notice would be sent unless she saw the specific notices and looked at each case. She said that the wording on "adverse action" notices, however, may cause some confusion. Adverse action notices inform enrollees that their benefits may be reduced or discontinued.
"(Adverse action) notices are used for numerous case changes but do not necessarily mean that coverage has been canceled. For example, with children we may issue an adverse action if a child is moving from Medicaid for Children to CHIP where they need to pay a premium in order to activate their coverage," Whaley said. "We are currently working on making our notices to participants more clear so that there is less confusion about what action was taken by the agency and what steps may be required of the participant."
In Missouri, 77% of coverage denials were for procedural reasons
During the pandemic, the Medicaid verification process was put on a three-year hold.
When the verification process started in June, about 1.5 million people, or roughly a quarter of the state, were receiving health care benefits from Medicaid. For those who enrolled during the pandemic, they may be navigating the renewal process for the first time. Now, more than 82,000 have been disenrolled, although 77% of those were denied coverage for procedural reasons.
Dr. Matthew Stinson said Jordan Valley Community Health Center has been working with about 50 people per week on Medicaid applications or renewals. Stinson is executive vice president of medical and behavioral health at Jordan Valley Community Health Center, which is a Springfield-based federally qualified health center with locations around the Ozarks.
Those who have been denied for procedural reasons have 90 days to complete the required paperwork and immediately resume coverage. They are eligible to reapply if they miss that 90-day window.
“Folks can always come in and reapply,” Whaley said. “Even for a number of the population that are eligible in Missouri we have what's called prior quarter coverage, which means that if they indicate on their form that they want us to look into that, then we potentially could cover the three months prior to their application date as well if they were eligible during those months.”
Whaley said that it can sometimes be hard to get in touch with some recipients, especially those who have not updated their address or phone numbers with the agency.
“One of the most challenging things is we understand that people who might use our services, a lot of times move around a lot,” Whaley said. “So if we don't have a good address for them, it's hard to send them information when we need to.”
Without reliable means of contact, it may mean that some recipients won’t even realize that they lost coverage until they try to use it.
“They might not realize it until they go in to get a medical procedure or go to the doctor,” Whaley said.
In an effort to prevent lapses in coverage like that, Stinson said the health center is trying to work ahead of enrollment deadlines.
"We’re working proactively with patients who are on our schedule to reach out to them ahead of time, to say, 'Did you know that your Medicaid has been terminated or is due to be processed here in the next 90 days, can we go ahead and set up a time to do that?'" Stinson said.
While the application or renewal process can be long and tedious, Stinson wants people to know that they don't have to navigate it alone. JVCHC has "a group of experts" patients can work with and computers set up at health centers so people can seek help while they complete renewal or applications.
"There is help; people don't have to be overwhelmed by (the process)," Stinson said.
Susan Szuch is the health and public policy reporter for the Springfield News-Leader. Follow her on X, formerly known as Twitter, at @szuchsm. Story idea? Email her at sszuch@gannett.com.
This article originally appeared on Springfield News-Leader: Missouri Medicaid denials largely due to paperwork issues

