3D-printed medical devices made by Materialise in Plymouth Township are saving lives
The tiny point of a laser zipped back and forth inside a machine, laying down layer upon layer of polymer, creating what will become a 3D-printed dental plate a surgeon will use to properly align the jaw of a patient with an overbite.
In another room, new metal 3D printing machines stood sentinel, waiting for digital instructions to print personalized titanium plates to help mend broken bones and orbital implants for patients who have suffered eye trauma.
It's all happening inside an unassuming building at the end of a tree-lined street in Plymouth Township, the North American headquarters of Materialise. The Belgium-based 3D printing company is improving — and saving — lives by making thousands of personalized anatomical models, implants and other medical devices using data from CT scans, MRIs and optical scans.
How a model of his heart saved a teenager
It's where a flexible model of the heart of a 16-year-old boy with a cardiac tumor was created.
"We worked with Cincinnati Children's Hospital on this," said Bryan Crutchfield, vice president and general manager for Materialise North America. "The young man's name was Brad, and he had a tumor for seven or eight years that they were monitoring. When he turned 16, they thought, 'OK, the tumor is invasive enough. He's old enough. We need to go in and take it out.' We helped them by creating this pliable model."
Crutchfield held a replica of Bradley White's heart in his hand, turning it as the doctors would have as they considered the best strategy for treatment. It showed exactly how the tumor was embedded in the heart tissue, and it also showed a serious flaw in their original plan for the teen boy's surgery.

"What they discovered through the model was that once they removed the tumor, there would not be enough tissue left to reconstruct his heart," Crutchfield said. "So, in his case, they didn't crack his chest open and surgically remove it. What they did instead was they went in minimally invasively and they did a thermal ablation."
The model helped the surgeons not only determine Brad's treatment plan, but also to explain the operation to Brad and his family.
"If a picture is worth 1,000 words, then a model is worth 1,000 pictures."
What's the one problem you would solve?
Dr. Glenn Green, a physician at C.S. Mott Children's Hospital in Ann Arbor, recalled his 3D-printing Field of Dreams moment.

It was a little more than a decade ago, and Green was talking with a colleague about what single medical problem they would solve if they could.
Green, who also is a professor of otolaryngology at the University of Michigan, said he wanted to help kids with a rare condition called tracheobronchomalacia, a sometimes-fatal condition that causes the structure of the windpipe and bronchial tubes to collapse, making it difficult for babies to breathe.
"When I was at the beginning of my career, we were losing kids — about one or two a year — due to this condition, and it was just really frustrating to watch these beautiful kids, and to get to know their families, then something would happen and they would pass away," said Green. "That was just devastating.
"It was a thought experiment: If you could fix one thing, what would it be? And I said, this is what I wanted to take care of."
Winning emergency FDA approval
Green and Dr. Scott Hollister, a biomedical engineer who now works at the Georgia Institute of Technology, came up with a solution: They would make a 3D-printed splint of dissolvable material called polycaprolactone, a biopolymer, that could be implanted in the airways of babies with this condition.
"If you can keep them alive, then get the trachea to the correct position, then they can grow out of it," usually by age 3, Green said. The goal would be to create a flexible scaffolding that would allow the child's own cells to grow into the splint to eventually support the windpipe and bronchial tubes on their own.
"We brainstormed," Green said. "We came up with a couple of different iterations. With 3D printing, you can really go through a lot of prototypes pretty quickly."

The device — made at a Materialise 3D printing facility in Ann Arbor — won special emergency authorization from the U.S. Food and Drug Administration to treat children who would die without the intervention.
And in 2012, Green was the first surgeon in the world to implant the device in a child — Kaiba Gionfriddo of Youngstown, Ohio.
'He wouldn't have survived without it'
Kaiba was just a few months old when he had surgery in 2012 at Mott.
"He wouldn't have survived without it," his father, Bryan Gionfriddo, told the Free Press on Friday. "We took the gamble and went to Michigan. Dr. Green explained everything, and showed us what he was going to do. He had a piece of the splint and showed us a model of his bronchotrachea and showed us how it was going to go on."
More: Doctors use 3D printer to custom make implant for baby
It saved Kaiba's life, Gionfriddo said, and today, his son is thriving. Kaiba will turn 12 in October. He is going to school, loves his pets and playing video games.
"He's doing real good," Gionfriddo said.
And so are the roughly 50 other children who've also gotten the 3D-printed tracheal-bronchial splints at the University of Michigan in the years since Kaiba became the first, Green said, noting that U-M is the only institution in the U.S. with special emergency authorization to use it.
"We'll have kids getting flown here from around the country," Green said. "Their families will come in and spend a month or more with us to have their kids taken care of. The parents are ecstatic that they're able to take their kids home afterward. Many of these kids had been in the hospital, the ICU (intensive care unit), their entire lives.
"They can grow out of it and then the splint dissolves and everything is perfect for them. Then, most of them live a relatively normal life."
The possibilities go from head to toe
That's just one of many stories about what can be done with medical 3D printing, Crutchfield said.
Materialise expanded its Plymouth Township facility over the summer, adding about 5,100 square feet and the capacity to begin metal 3D printing using titanium powder.

For now, the site's nearly 100 workers mostly build patient-specific plates to help surgeons hold broken bones in place, craniomaxillofacial implants and cutting guides. But eventually, he said, it could add more personalized 3D metal printing for hips, shoulders and cranial implants, which are now made at the company's headquarters in Leuven, Belgium.
By growing its production capacity in the U.S., Materialise can make personalized medical devices and ship them to hospitals and medical clinics in North America much more quickly.
And in medicine, turnaround time is important.
"It's shortening the lead times by two or three days," Crutchfield said. "A lot of it is still elective surgery, not really trauma because turnaround time for trauma is a bit quick for 3D printing. But that's what we're working toward. We're trying to squeeze those lead times so we can better address the market with our partners in the orthopedic industry."
The Plymouth Township site also is continuing its work in plastics 3D printing, making surgical guides that fit over bones to help doctors properly align them during surgery, showing them where to cut and where to screw in pins.
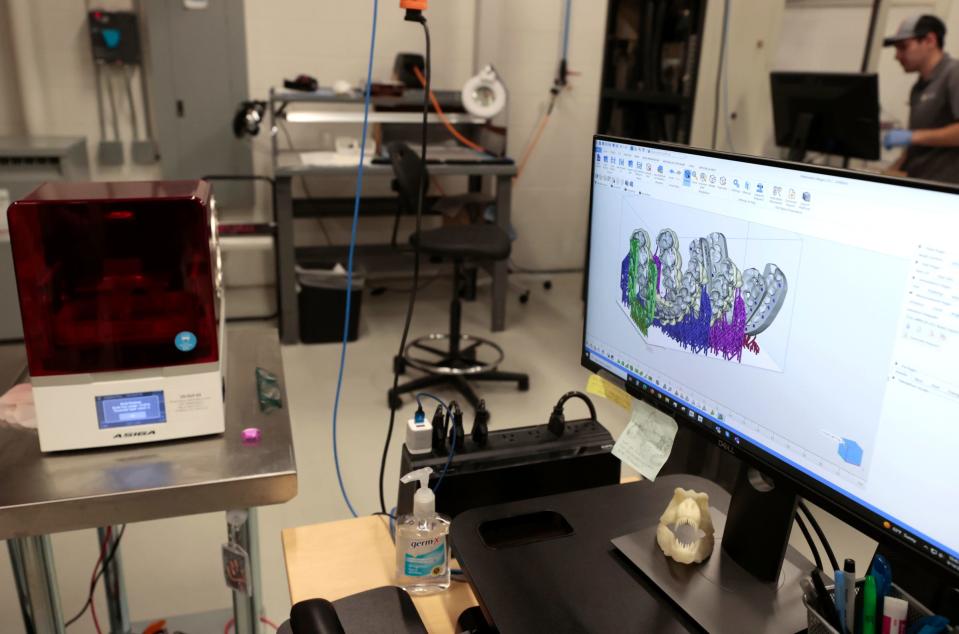
"We’re showing them exactly where the cuts need to be made and exactly where the guides should fit. And they will only fit the patient in that way," Crutchfield said. "These systems improve precision and take it down to plus or minus 3 degrees of variation.
"We’re literally taking people who have never walked in the correct plane before and they’re correcting people who are bowlegged or knock-kneed. Many of them are, for the first time, going to be walking correctly."
It shortens the time patients are in the operating room, he said, and improves recovery time, too.
"The more precise and tight fit you get with the implants, the faster the healing process will happen," Crutchfield said.
Contact Kristen Shamus: kshamus@freepress.com. Subscribe to the Free Press.
This article originally appeared on Detroit Free Press: Materialise in Plymouth Township saves lives with 3D-printed devices

