What’s affecting your health in Miami? Hospitals did a survey to help tackle the issues
Better access to care, a need for more mental health resources, and a desire for more financial stability are the top three concerns in Miami-Dade County, according to a new assessment conducted by hospitals in the county.
Jackson Health System, Miami-Dade’s public hospital network, conducts this assessment every three years with other hospitals to get a better understanding of what is affecting people’s health, what is stopping people from getting care, and what can be done to help people live healthier lives in Miami-Dade County.
As part of the 16-week assessment, which began in February, officials reviewed data, held focus group sessions, conducted a community health summit in July with “community stakeholders” and sent out surveys to Miami-Dade County residents, providers and employees as part of their deep dive.
This year’s assessment was done in partnership with Miami-Dade County, Nicklaus Children’s Hospital near South Miami, Mount Sinai Medical Center in Miami Beach and the University of Miami Health System. It will help craft hospital strategies and initiatives to improve care through 2027.
And while COVID-19 no longer made the list now that the pandemic has subsided, it’s not just chronic conditions like heart disease and diabetes that made the cut. Longstanding social issues — economic and social factors that can affect health — such as a lack of affordable housing, food insecurity and access to health insurance have continued to rank high on people’s minds.
Let’s dive into the report:
Top health needs in Miami-Dade County
Of the 20 health issues identified, community stakeholders — 120 people representing organizations that help the community such as Camillus House, Feeding South Florida, United Way Miami, The Children’s Trust and the Florida Department of Health in Miami-Dade — were tasked with identifying the top eight priorities.
The priorities were ranked using the following criteria: Magnitude (how big and widespread is the problem?), seriousness of the consequences (what happens if the issue is not made a priority?), equity (does this affect certain groups more than others?), and feasibility (how preventable is the problem and is it addressable?).
The top eight priorities:
▪ Access to healthcare
▪ Mental Health
▪ Income equality/financial stability
▪ Housing
▪ Access to affordable health insurance
▪ Chronic diseases
▪ Nutrition/food insecurity
▪ Maternal and child health
READ NEXT: Medicare enrollment is now open. What coverage questions do you have?
An overview of Miami-Dade
As part of the assessment, participating hospitals sent out a survey to employees and providers. The report says 885 employees and 147 providers participated, with the majority describing the overall health status of Miami-Dade as “fair or poor.”
But there is some good news — the report says people who live in Miami-Dade can expect to live about three years more (about 81 years of age) then the average U.S. resident (about 78 years of age) based on 2018-2020 National Center for Health Statistics data.
Here’s what else survey responders said:
▪ Most prevalent chronic diseases in Miami-Dade: High blood pressure, diabetes and obesity. Heart disease is the leading cause of death in the county, followed by cancer, COVID-19 and stroke.
▪ Top three issues that affect people’s health: Access to affordable health insurance, healthcare services and fresh and natural food.
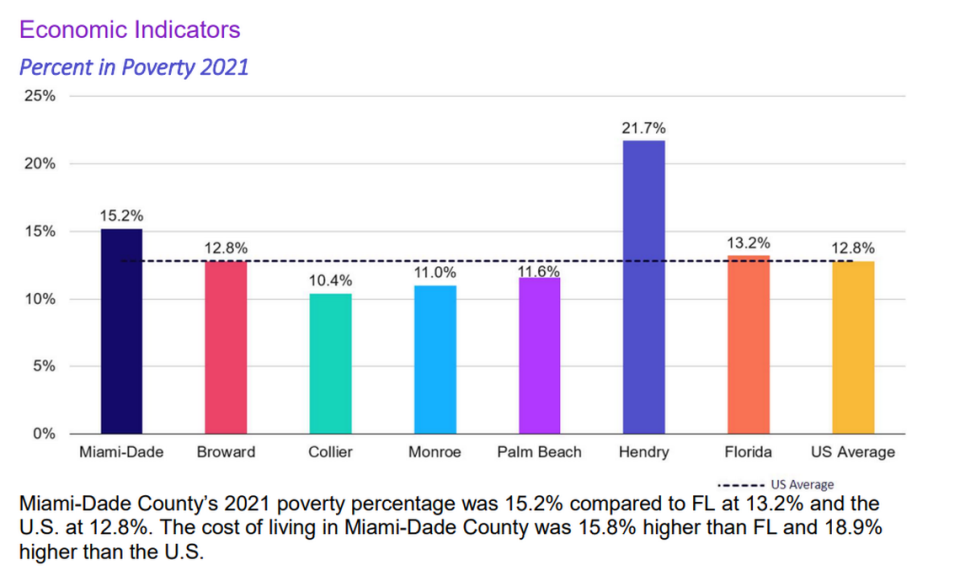
▪ Top three social determinants of health: Poverty (financial stability), a need for available and affordable housing, jobs. The cost of living in Miami-Dade, for example, is 18.9% more expensive then the rest of the U.S., with the poverty rate (15.2%) also higher than the U.S. (12.8%), according to the report.
▪ Top three issues for children: Physical activity, healthy diet and obesity.
▪ Limitations: The report notes that while it’s a comprehensive overview of health in Miami-Dade, its unable to “measure all aspects of health in the community” nor can it adequately represent every possible population, which could limit the ability to assess the needs of everyone in the community such as those who don’t have a home.
READ MORE: Want to live to 100 or older? Experts in Miami suggest taking these five steps now
Do community needs differ depending on where you live?
Surveys were also sent to 800 households across the county this year to see what needs different parts of the county have.
The results:
▪ Northwest Miami-Dade “struggles more with access, gaps in insurance coverage, asthma, healthy weight, financial stress, fresh food availability, stress, smoking and vaping, illicit drug use, lack of access for pediatric care, and lower HPV vaccinations.”
▪ South Miami-Dade “struggles more with available healthcare services, physical exams, higher ER visits, gaps in insurance coverage, COPD, physical pain, obesity, domestic abuse, financial security, food insecurity, poor mental health status, receiving mental health treatment, lack of mental health access, smoking, illicit drug and opioid use, negative impact of substance use, and pediatric autism spectrum disorder.”
▪ Central Miami-Dade “struggles with neighborhood safety, living conditions, exercise and drinking.”
▪ Northeast Miami-Dade “struggles with the fewest issues of all the segments, leading in only high cholesterol and pediatric asthma.”
READ NEXT: Which states have the best and worst healthcare systems? See how Florida ranks
Do needs differ by ethnicity and race?
The household surveys also give a glimpse into what the needs are, depending on a person’s race and ethnicity:
▪ Hispanics “struggle with access to care, gaps in insurance coverage, financial stress, higher food insecurity, higher stress, higher fair or poor mental health, higher smoking and vaping, higher use of illegal drugs,” and are most affected by drug use, the report states.
▪ Whites are more at risk of cancer and heart disease diagnosis, have a higher use of opioids and are more likely to have a child on the autism spectrum, according to the report.
▪ Blacks are more at risk for chronic conditions such as stroke, diabetes and high blood pressure, often are higher users of illegal drugs, and are more at risk for domestic abuse, according to the report. Blacks also often live with social determinants, such as financial stress, poor housing conditions, more food insecurity and less safe neighborhoods, the report states.
READ MORE: With fentanyl use on the rise, Miami schools are taking steps to cut risk. What to know
Read the report
The report has a lot of data, and a lot of other interesting findings. Read it below:

