Antibiotic-resistant bacteria are killing us. Here's how we can defeat these 'superbugs.'
By some estimates, antibiotic-resistant bacteria are already killing more Americans than car accidents and even opioid overdoses.And the situation is getting worse.
In a report this month, the Centers for Disease Control and Prevention estimates that more than 35,000 Americans die from drug-resistant infections each year. Yet for a variety of reasons — including that hospitals often report cause of death as the illness that first brought a patient to the hospital rather than the resistant bacteria they acquired there — the CDC’s estimate is likely still too conservative. Other estimates place the number of annual deaths in the U.S. at 100,000 or more.
Most of modern hospital medicine relies heavily on effective antibiotics, and drug-resistant infections are rampant in these settings. Particularly susceptible are people with compromised immune systems such as premature babies, transplant patients and people getting cancer chemotherapy. Also at risk are those with implanted devices, people with diabetic foot ulcers and anyone having surgery.
Heed the lessons of evolution
Yet solutions — simple in principle — are possible. And they don’t require spending exorbitant amounts of money on new drugs that will fail in the manner of their predecessors. Instead, we can apply what we know about evolution to stop resistance.
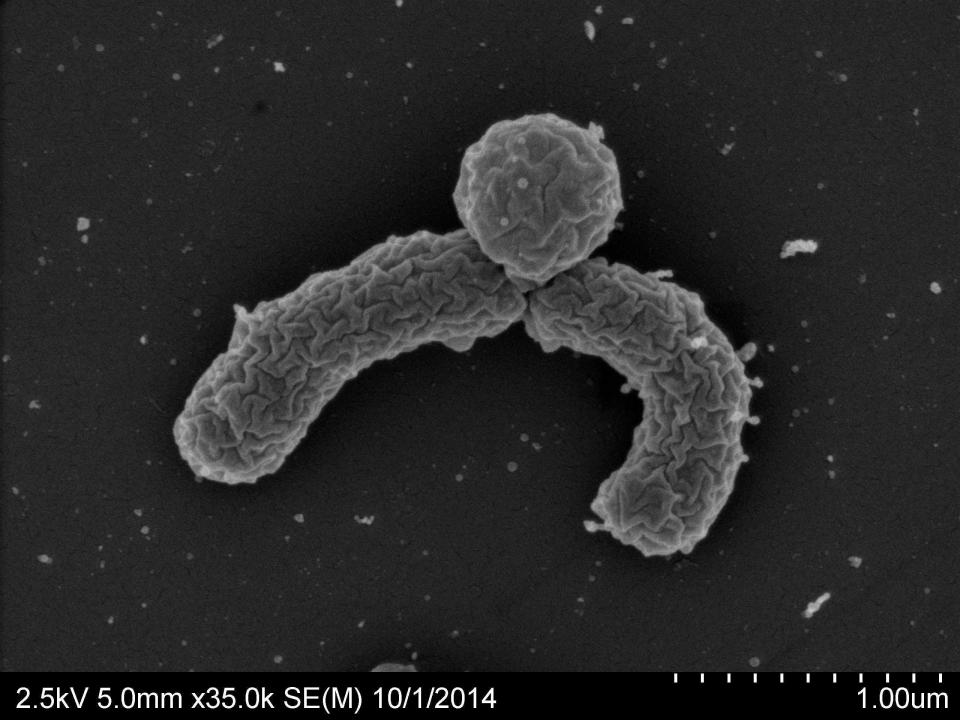
Antibiotic resistance arises when genetic changes in their DNA enable some bacteria to survive drug exposure. With their drug-sensitive competitors killed off by the antibiotics, the resistant bacteria can flourish and go on to cause illness despite the antibiotic. And, just like any other germs, these resistant bacteria can spread to other people. This process is textbook Darwinian evolution by natural selection.
A guiding principle should be to avoid, whenever possible, taking actions that will further drive the evolution of resistance. But there is an urgent need to figure out how best to do that. More research is needed to test potential solutions.
For example, rather than expecting drugs to do all the work, we could examine, for those with healthy immune systems, using just enough drug to knock bacterial populations down so our immune systems can gain the upper hand and finish the job. The medical orthodoxy that pushes patients to complete drug courses even when they no longer feel sick can promote the very evolution it is intended to prevent. That’s because longer drug courses can kill off the beneficial bacteria that could otherwise outcompete resistant ones.
Where's the oversight?: Unregulated vaping spawns new teenage nicotine addicts. And now adult vapers are dying.
Another approach is to use combinations of antibiotics to treat infections. Combinations can halt the evolution of resistance simply due to the sheer unlikelihood that a single bacterium will develop resistance mutations to numerous drugs at once. The strategy is well-established in diseases such as HIV, tuberculosis and cancer.
Vaccines offer yet another solution. They’re much more evolution-proof than antibiotics, in some cases providing sustained disease control for many decades.
We must preserve precious antibiotics
A few years ago, a physician at a hospital in Michigan asked for my advice. His patient had an Enterobacter infection, and he’d tried antibiotic after antibiotic to treat her—without success. With only two drugs left, I suggested he use both simultaneously. My thinking was that since the drugs had different modes of action more mutations would be required for the bacteria to generate resistance to both drugs.
At the time, however, there wasn’t enough justification to go with my theory. So the physician went with best practice — try one antibiotic until it fails, then switch to the other. The patient died, not from the heart failure that brought her into the hospital in the first place, but from the evolution of drug resistance among the bacteria in her body.
I lost my son to the opioid crisis: Here's the right way to spend billions in settlement money
Could we have staved off that evolution for longer? More laboratory studies are needed to better understand how to manage the evolution of potentially dangerous bacteria. Then we need to apply what we learn to humans, carefully. It's likely that no one generic solution will emerge, but I am confident we can do much better if we go after the evolution.
If scientists, the medical community, and funders don’t act now to address the problem of antibiotic resistance, we will all suffer serious consequences. But I am optimistic that so long as we apply the lessons of almost two centuries of research about how evolution works, we can effectively steward our precious antibiotic resources and save countless lives.
Andrew Read is Fellow of the Royal Society of London, director of the Huck Institutes of the Life Sciences, Evan Pugh Professor of Biology and Entomology, and Eberly Professor of Biotechnology at Penn State.
You can read diverse opinions from our Board of Contributors and other writers on the Opinion front page, on Twitter @usatodayopinion and in our daily Opinion newsletter. To respond to a column, submit a comment to letters@usatoday.com.
This article originally appeared on USA TODAY: Superbugs resistant to antibiotics are killing us but we can beat them

