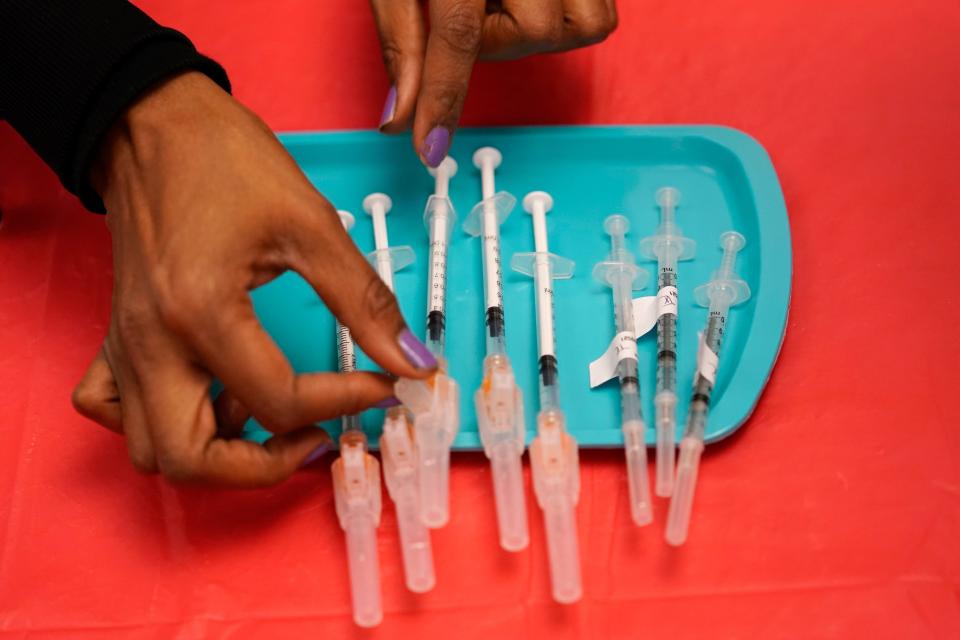
‘We’re Apollo 13-ing this vaccine rollout’
In Will County, Illinois, just outside Chicago, health officials knew a deluge was coming once the first COVID-19 vaccine was authorized. They started working 12-hour days and weekends.
“I was getting the kids to bed and jumping back on the computer till 9 or 10,” said Katie Weber, the county health department’s emergency response coordinator.
Weber had three enormous tasks ahead of her. She and her team had to make sure health care providers in the county were correctly linked to the state’s vaccine ordering system, figure out who was eligible to get vaccine first and where they were, and coordinate every one of her county’s health care workers, law enforcement officers and teachers into vaccination clinics. And she had to deal with dozens of companies clamoring to get their employees vaccinated.
“When you’re a local health department in the midst of a pandemic and have been going for eight, nine months, and you’re told you’re going to have the vaccine next month ... that’s a huge task,” she said.
Like many other health officials faced with the daunting duty of vaccinating their corner of America, Weber had to piece together an information technology system in the face of unstable vaccine supply and strained staff and resources, with little time to plan, after waiting on state and federal health authorities for answers about vaccine supply and guidelines.
Though the federal government spent millions on vaccine scheduling and supply management programs, it was of little use to local officials, who scrambled to come up with systems on their own.
“I feel like we’re Apollo 13-ing this vaccine rollout,” said Becky Colwell-Ongenae, the county’s geographical information system manager, who developed maps and tools to help Weber pinpoint priority populations and identify prospective vaccination sites. “I got a plastic bag and some tweezers, and I gotta moonshot home.”
Far from the fancy databases big companies might use, Webster and her team of a dozen county employees relied on Excel spreadsheets and an email program that balked every time she tried to send more than 500 messages at a time.
“I hate to be callous about it, but we’re sort of seeing you get what you pay for," said Rebecca Coyle, executive director of the American Immunization Registry Association. "If you don’t have a funded public health infrastructure, you’re going to see these kinds of problems.”
What is remarkable about the rollout of COVID-19 vaccine to the entire nation, said those who work in the field, is not the problems that occurred but that it worked at all given the chronic lack of funding.
“If you go to any health department, you could be stepping back technologically five or 10 years, from the version of the software that’s used to the machines they work on," said Tiffany Tate, executive director of the nonprofit Maryland Partnership for Prevention. "Everything is old and outdated.”
Homegrown IT solutions
In Washoe County, Nevada, officials said they were short-staffed and hampered by communication delays from the state. They cobbled together data and logistics solutions to get vaccines into arms.
“The state of Nevada kind of dragged their feet on a lot of these things. We struggled for a long time with spreadsheets,” said Gary Zaepfel, a systems developer coordinating the information technology projects for the county’s COVID-19 vaccination rollout.
Zaepfel and his team came up with solutions to connect appointments, employers and providers with the county’s health district. They use the software system Accela for appointments and custom-built software that lets companies apply as essential businesses and receive prioritization. Those companies are then approved by the health district.
In Alaska, the Anchorage city government built web applications to lower the barrier to finding vaccine appointments. Many of the state’s larger vaccination sites used PrepMod, a vaccination management system that ties into state immunization registries and allows the public to book appointments, and the city fielded a flood of calls from disappointed residents.
“In January, we started getting complaints from senior citizens that they couldn't find an available vaccine appointment,” said Ben Matheson, a data analyst on the city’s innovation team. As is common elsewhere, appointments were posted across pharmacy, hospital, government and supermarket websites. Even for the tech-savvy, jumping between many websites to find an appointment was an uphill battle.
Matheson built a simple website that pulled together vaccine appointment information from several sources and updates dozens of times a day. What was a weekend proof-of-concept project has become a “power tool” for the city’s COVID-19 call center, he said. He built another bare-bones website that finds available coronavirus testing appointments across the city.
“That was a blessing for us that we could make a dead simple website that works on phones and gets you to what you want," Matheson said. "We should be doing everything we can to get people a vaccine appointment.”

‘Mired in the process’
Not every city and health office has the tech savvy or resources to build software and IT solutions to lower the barrier to getting vaccines. Though every state has a license for mapping software from Esri – which rolled out several tools such as data dashboards and survey forms to assist health officials in the vaccine rollout – not every health department or municipal government has the staff to employ that technology or tailor it for local needs.
“My general frustrations are that we’re underfunded in public health but we’re asking people to know a lot and do a lot,” said Este Geraghty, chief medical officer at Esri and a former official at California’s Department of Public Health. “It’s a lot harder than it looks to put these things into motion.”

Geraghty ran into these issues firsthand when building product demos for Georgia and Alabama to help them identify at-risk populations and move around vaccine inventory. When the Centers for Disease Control and Prevention released its vaccination playbook in October, the vaccination phases and process looked fairly straightforward, she said. “But then we tried to operationalize it as we built the demos, and we said, ‘Oh, no, it’s not.’”
States were left to figure out their own systems without much centralized help.
“Certainly it would have been helpful to have had more federal guidance,” Geraghty said. “Having every state have to figure it out on their own was really a disservice. It’s how people got mired in the process.”
Federal funding unclear
The federal government promised to do more to fund public health in the wake of the pandemic. The American Rescue Plan dedicates billions of dollars – mostly to the Department of Health and Human Services and CDC – to support COVID-19 mitigation and vaccination activities and other public health programs. Some of that money is supposed to go to states.
It’s not clear whether that funding will trickle down to county and local health departments, of which there are nearly 3,000, says Lori Tremmel Freeman, CEO of the National Association of County and City Health Officials.
SUBSCRIBE: Help support quality journalism like this.
“We have no idea how much money is going to reach locals even out of the American Rescue Plan,” she said. “It’s going to states and the five largest cities. There’s no language that mandates that money gets to the local health departments or the communities at all. Even the supplemental funds Congress has approved in the last year have not in all cases reached the ground level where the fight occurs to mitigate this disease.”
Local public health departments are seeing their budgets contract. Those departments have lost 20% of their staff in the past decade, said Freeman, citing a survey the NACCHO routinely runs.
“Our health officials take full responsibility and accountability for their communities," she said. "So it’s really a terrible message we’re sending when we don’t give them the tools they need to take care of them.”
Learning lessons
COVID-19 vaccination efforts were going to be a huge logistical challenge in any case, but they hit a decentralized, chronically underfunded public health system that struggled to keep up.
“It really is amazing, given where we were, that the rollout has gone so smoothly,” said Maryland Partnership for Prevention's Tate, who developed the vaccine management system PrepMod.
The system is used in at least some counties in almost every state by more than 55,000 people in public health departments, clinics and medical offices.
Its introduction wasn’t without its stumbles. Most officials using PrepMod signed contracts that allotted them a certain number of simultaneous users. That worked fine when people were signing up for flu shots but went out the window after COVID-19.
“Take California," Tate said. "They were supposed to have up to 6,000 users in the system at any one time, and now they’re at 20,000. They’re adding about 1,000 a week.” On the back end, that meant adding cloud computing space to handle the ballooning numbers and staff on the help desk.
PrepMod runs the Massachusetts state system, which slowed to a crawl last month when 9.4 million people tried to sign up in a five-hour period, Tate said.
“It’s like someone announced that Beyoncé, Bruce Springsteen, Taylor Swift, Justin Bieber and Tim McGraw were all coming together to do one concert together,” she said. “It was unprecedented demand.”
Many states used PrepMod instead of the original federal scheduling program, VAMS, or Vaccine Administration Management System. It was supposed to be a free vaccine scheduling, inventory and reporting program, for which the CDC paid the consulting firm Deloitte $44 million.
VAMS suffered from multiple problems, including randomly canceling appointments.
“That was the system everybody hated," said Cimarron Buser, president and CEO of the Appointment Scheduling & Booking Industry Association. "The people who built the software never thought about what happened when there wasn’t enough vaccine.”
Tiberius, another national supply chain management system released by the federal government to aid in the COVID-19 vaccine rollout, largely failed to live up to its promise. Many states found Tiberius too complicated or irrelevant, a USA TODAY investigation found, relying instead on their own data and systems. Few counties have access to Tiberius.
Coyle, of the American Immunization Registry Association, said that "once the dust has settled," the country must take stock of the rollout – and learn from it.
“What we really need is a weeklong hash-out, a chance to sit down and debrief with everyone to figure out exactly what happened,” Coyle said. “Nobody has the time to do that right now. But this, too, shall pass. Eventually, we’ll pause when this is over and capture what worked and what didn’t.”
This article originally appeared on USA TODAY: COVID vaccine: How local officials used tech to distribute vaccine

