Arizona senior living facilities are often understaffed, endangering workers and residents
At Austin House in Cottonwood, there was little time for introductions.
So when caregiver Susan Severe met her newest resident in the winter of 2021, a co-worker simply told her, "He's not nice."
She knew he'd been a loner. He was in his 70s and was suffering from dementia.
"I knew he cursed a lot," she said.
That was about it.
Over the next month she grew accustomed to his outbursts. One day he wandered into the med-tech room and knocked over shelving units loaded with bandages, socks, briefs and gloves.
Management moved him into a unit that specializes in behavioral issues. But that didn't make much difference.
Austin House — now under new ownership and called Verde Valley Assisted Living — has three sections. One is general assisted living. Another is for people with dementia or cognitive issues, and the third is for those with behavioral issues separate from dementia.
Severe never knew which unit she'd have to work until she clocked in for the day.

On Jan. 11, 2021, she started the day in the behavioral unit.
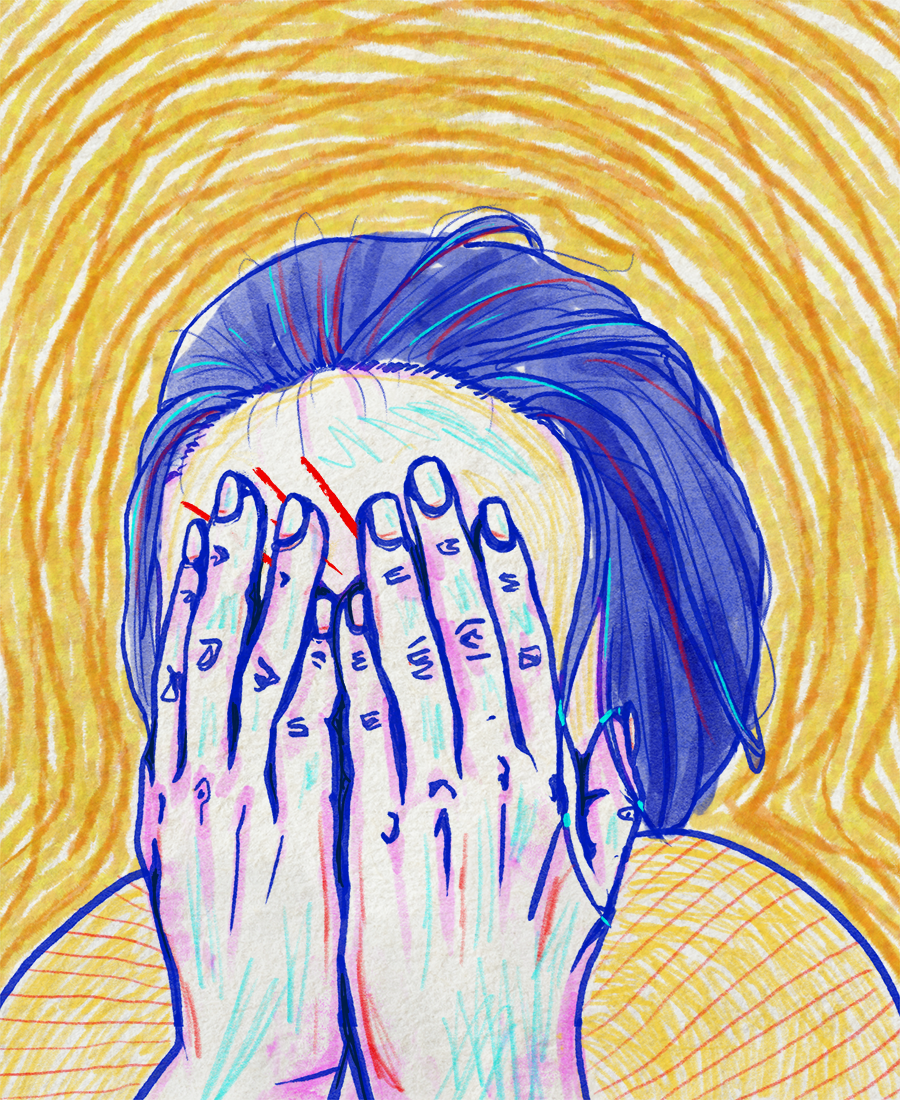
She ended the day on a stretcher, blinded in one eye, having wet herself from terror.
Caregivers at assisted living facilities and nursing homes generally work for minimum wage or slightly more. They are often single moms, immigrants, minorities or even seniors themselves.
In Arizona, they have no union to leverage better working conditions.
The whole industry operates on their backs.
Their job isn't easy. They must change adult diapers, feed and bathe residents. They also make sure residents get prescriptions and, depending on their training, provide medical care.
If they make mistakes, the results can be deadly.
The pressure is exacerbated by staffing shortages and insufficient training, which put both residents and caregivers themselves in danger.
Stressed out, employees may miss call lights, mess up residents' medications or miss opportunities to prevent violence. Even well-intentioned caregivers can interact with residents in ways that leave one or both parties uncomfortable.
Caregivers shoulder insults and slights — sometimes racist or misogynist comments — and occasionally they must find ways to break up fights.
Or, like in Severe's case, lack of support leaves them vulnerable to serious injury.
The Arizona Republic found about 30 police reports documenting when residents physically took out their frustrations on caregivers, inflicting injury in more than half of these incidents over the past three years. The actual count is likely much higher. The Republic does not have records from every police department in the state and not every attack at senior care facilities is reported to law enforcement or regulators.
"Caregivers need help," Severe said. "We are not protected."
‘Low staff is definitely a problem’
The overwhelming majority of senior living facilities across the country are understaffed. That’s the way their owners choose to operate, researchers say.
Staffing is a major cost and a critically important determinant of quality care. When a company tries to increase profits by reducing staff, dangers to residents and their caregivers grow.
But company finances are rarely transparent, obfuscating how much owners make from their senior living operations — and to what extent their profits are inflated by low staffing at facilities.
Nursing homes, which provide both long-stay care and short-term stops for people who need rehabilitation after illnesses or injuries, are required to provide financial and ownership information to the Centers for Medicare and Medicaid Services — something assisted living facilities don't have to do.
According to that data, less than half of the 129 nursing homes analyzed by The Republic made a profit from services provided to residents in 2021. But that number doesn't tell the whole story, some academic researchers say because the regulations that govern nursing home financial reports allow companies to cloak how much money they pull out of their facilities.
Some nursing home owners draw money out of their facilities and into other companies they own to make their profits look lower so nursing homes can ask for more money from Medicare and Medicaid, according to Charlene Harrington, professor emerita of sociology and nursing at University of California-San Francisco.
"The standard practice is to set up all these related-party companies," Harrington said. "The money is just being siphoned off. And it looks like an expense on the cost report — but it's actually a profit to the parent company."
Those profits aren't always visible, but even when they are, it's unclear whether those dollars go toward increasing facility staffing levels.
The Ensign Group is one of the largest publicly traded nursing home chains and owns about 30% of Arizona's nursing home beds, a Republic analysis revealed. Ensign's revenues steadily increased from 2007 to 2020, and nearly all of the money it made during that time period came from its nursing homes, according to a recent study Harrington co-authored.
But that study found that on average, Ensign's nursing homes failed to meet minimum suggested nurse staffing thresholds from 2020 to 2021. The thresholds were established by a 2001 study for CMS that showed how staffing levels impacted the quality of care provided to long-stay residents.
Only two of the more than 30 nursing homes Ensign owns in Arizona met the threshold for registered nurses in the first three quarters of 2022. None met the threshold for certified nursing aides, according to an analysis by The Republic.
Ensign, like other big nursing home owners, has a financial stake in many companies and corporate entities, hundreds of which it used to own and operate more than 200 senior care facilities across the country in 2020. Some of those companies provide services like accounting and payroll to Ensign’s nursing homes. It’s not clear from Ensign's financial statements how much money its service-providing companies make from its senior living facilities.
Barry Port, chief executive of the Ensign Group, said each nursing home affiliated with his company has leaders at the local level who operate in the way that best serves residents, employees and community.
"Staffing is very much facility specific without a 'one-size fits all' approach," Port stated in an email. "Every facility affiliated with The Ensign Group has a clinical and operational leadership team who are directly responsible for … making their own dynamic assessment of staffing levels on a daily basis. This approach has led to superior outcomes by our affiliates in the State of Arizona."
Port added that any statements suggesting the Ensign Group siphons money from facilities to bolster company profits instead of improving staffing levels and resident care are “categorically false.”
The Republic's investigation did not uncover records suggesting that Ensign required its properties to pay inflated rents or purchase supplies and services at inflated prices from its subsidiaries — practices employed by some companies owning nursing homes.
Ensign's Arizona nursing homes aren't the only ones that failed to meet minimum suggested CMS staffing thresholds.
Roughly 80% of nursing homes in the state failed to meet the minimum threshold for certified nursing aide staffing in each of the last 5 years, according to a review of staffing levels by The Republic. More than 60% failed to meet the threshold for registered nurses over the same time period.
No similar statistics are publicly available for assisted living facilities at the state level. But the National Center for Assisted Living found that more than 60% of the 120 providers it surveyed last June faced moderate to high staffing shortages.
Academic researchers say the main reason for the shortages is that companies that own senior living facilities are bent on maximizing their profits.
"A nursing home can save as much as $1 million a year on staffing — that's one of the main ways they can maximize their profits, so there's a tremendous pressure to do that," Harrington said.
A 2021 study showed that when private equity firms buy nursing homes, staffing declines and deaths rise. The rate of patient deaths during a nursing home stay and the following 90 days was 10% higher at facilities owned by private equity firms than at nursing homes overall. The study also showed that residents’ mobility declines after an acquisition, and they experience more pain.
Industry trade groups that represent nursing homes, however, say that staffing shortages aren't caused by the unbridled pursuit of profit but rather by a lack of qualified and interested candidates to fill openings.
"This work is not the most glamorous work," said Jen Bonilla, former executive director of academic operations at Arizona Nursing College’s Phoenix campus. "It's not going to always attract top talent who may desire to go work at Mayo Clinic."
Unlike nurses in outpatient clinics, staff at senior care facilities often see patients they’ve taken care of for months — even years — die. That emotional aspect can heighten burnout or deter some nurses from working in senior care settings, Bonilla said.
"Grief is a significant issue for people who work in those environments," she said. "In many cases those are their friends, they see (residents) like their grandparents or their parents, then who are passing."
Bonilla added that an ongoing national shortage of nurses, driven in part by a lack of qualified educators, only makes things harder.
And the pandemic didn't help. The senior living industry was thrown into chaos in 2020. Occupancy levels plummeted, and finding willing workers — already a concern before the pandemic — became even more difficult. Facilities had to scramble to provide care.
More than 300 facilities nationwide closed their doors in the pandemic's first two years, according to industry advocates.
"We've closed one of our two skilled nursing facilities because of staffing shortages," Donna Taylor, former chief operating officer of Lifestream Senior Living in Youngtown, said in a statement issued September 2021. "It was heartbreaking. Most of our workers stayed with us through the really tough times last year. But this is hard: our people are tired. We’re seeing staff leave now."
Caregiving at a facility is often physically demanding, exhausting work — and nursing home positions typically pay less than jobs in hospital care settings, according to wage estimates published by the Bureau of Labor Statistics.
State estimates from the Bureau of Labor Statistics for May 2021 reveal that the average annual wages for home health and personal care aides and nursing assistants working in Arizona were $29,440 and $34,610 respectively.
In Arizona, housekeeping cleaners, restaurant hosts, and receptionists were estimated to make roughly the same amount.
"Unfortunately, we don’t have a magic wand," said Kris Woolley, founder and CEO of Mesa-based Avista Senior Living. "We can't just pay people whatever we would like to or whatever they would like."
But, he said, facilities must do everything they can to create an environment where employees are well-compensated, feel heard and can sustain a good work-life balance.
"No one is put on Earth to work for our company or any company, for that matter," Woolley said. "We have to be competitive in all aspects of our employment: salaries and wages, benefits, flexibility in the schedule, and treating them with dignity and respect. If we don’t do those things, they are going to find work somewhere else."
‘They don’t teach you much’
Susan Severe worked most of her life in grocery store delis. She decided to try something new when she moved to Cottonwood from Washington. Her ailing mother wanted to move south for the blue skies. Severe followed to care for her.
By 2018, Severe needed to make more money than her Social Security offered so she applied for a job at Austin House.
After getting a fingerprint clearance card and a background check, she was hired. She'd be paid $10 an hour, part-time.

Severe hadn't worked in senior care, but she has a natural way of comforting people and effortlessly stirs up laughter.
"Deli to caregiver — yeah that's a big difference," she told Republic reporters. "I can't make sandwiches out of them."
She figured she'd be given more training before she hit the halls at Austin House.
That was not the case, she said.
Severe shadowed other employees for about a week or two and then she was on her own.
"To tell you the truth, they don't teach you much," she said. "You just go."
The facility changed hands in March, and a spokesperson for the new management said staff assigned to work with the behavioral residents receive weekly training.
"Our facility's principal objective is, and will continue to be, providing the best care for our patients and their families, and providing a safe environment for our patients and staff," said Dan Kramer in an email. "In furtherance of that objective, we believe we have appropriate training programs and mitigation practices in place to minimize the risk of incidents of the kinds you have described."
Kramer said he could not speak to the facility's practices, procedures or personnel when Severe worked there, but he told The Republic that the weekly training started years prior to 2020.
When asked for copies of that training, Kramer declined, saying he wouldn't want to share "any information that we could not be absolutely certain was complete."
"They're so full of crap," Severe said in response. "Oh, they're so full of it."
Severe said she worked nearly a year before getting her caregiver license. The facility didn't make her do that, she said. They just told her she could get paid an extra dollar per hour if she did.
Waiting for hours for pain meds
When senior living facilities are short on staff, residents suffer. Busy caregivers can be brusque, and sometimes, brusque turns to brutal.
State reports document residents complaining to government inspectors that facilities are so short-staffed that call lights go unanswered for more than an hour at a time.
Those call lights often signal excruciating physical discomfort.
Residents wait in pain for medications, food or water. One woman described waiting for three hours for someone to close the window in her freezing room. She said she watched a gust of wind blow the calendar off her wall.
Some residents lie in their bowel movements for hours at a time. Others fall when attempting to get to the bathroom by themselves.
Residents at Haven of Sierra Vista complained that they didn't get regular showers — sometimes going two weeks without being able to bathe. One resident "was observed to have a white flaky and crusty appearance on his face, scalp and neck, and very dry flaky skin on his arms."
Soon short-term problems turn into chronic issues. Pressure ulcers don't heal. Muscles grow weaker without access to regular mobility exercises.
And when those problems are multiplied by dozens of residents, it means that staff is "working against the odds," as one nurse at Life Care Center of Tucson put it in a statement of deficiency interview.
"It feels like it never stops," another nurse said of the unceasingly demanding working conditions. Management had been informed of the problem, he added, "but nothing ever changes."
But sometimes, beyond issues worsened by neglect, caregivers actively hurt residents.
Seniors have complained more than 30 times to police about their rough handling over the past three years, according to The Republic’s review of police reports. Residents say that caregivers bang their body parts on beds, wheelchairs and rails.
One resident at Palm Valley Rehabilitation & Care Center (now known as Palm Valley Post Acute) in Goodyear said that a nurse hurt her by pressing a urinal device against her vaginal area.
"Do you have to pee or not?" the nurse said, according to the police report.
When the patient said she was being too rough and it was hurting, the nurse allegedly replied, "I don't care if it hurts or not."
The nurse explained in an interview with police that the urinal device required some degree of force to ensure a proper seal and insisted that she did not "intentionally or recklessly cause harm to her patient."
Tasks like these may challenge even the gentlest of caregivers. And not all caregivers are gentle.
One caregiver strapped a resident to a gurney so tightly that the man, who had a fractured clavicle, screamed out in pain, according to a police report.
Another woman told her daughter that a caregiver had tried to pull her out of her bed by her arms to give her a shower. The woman already had a broken collar bone and the caregiver's actions opened a cut on her left hand. When the woman’s daughter came to visit a short while later, she found her mother with a large bandage on her hand. Her bed was in disarray and there was blood on the sheets. The caregiver was fired.
In one extended case of residents suffering both neglect and abuse, Mesa police responded to more than 60 calls over a six-month period between August 2020 and January 2021 at the Ensign affiliate Montecito Post Acute and Rehab Center in Mesa — nicknamed the "Piss Palace" by firefighters called to the scene because of the overwhelming stench of urine.
A policeman responding to an incident in early 2021 "observed the rooms were extremely dirty and cluttered with objects." A large number of call lights were illuminated.
When he met up with three employees and asked to see a resident who had dialed 911, none of them knew who she was. The officer had to tell them that she lived in room 132, which turned out to be directly across the hall from where they were standing.
Upon entering the room, the officer noted a strong scent of urine. He said the woman’s sheets were wet in spots. She told him she wanted to leave the facility because the place was "horrible," no one ever came to her room and she didn't even have a call button.
A bedpan with urine in it sat on the floor at the edge of her bed.
In the same report, the officer listed a litany of complaints that had been filed in recent months. They included claims that money and belongings had been stolen from rooms; that a resident was not being fed or bathed; that a man had gone missing; that someone's mother had been given the wrong medication; and that staff had not been answering the phones.
There was also a call about a resident falling out of a third-story window, but she was moved back to her bed before emergency responders arrived, against the direction of the 911 call takers.
She often felt unsafe
Despite her best efforts to understand the plight of residents, Severe often felt unsafe at Austin House.
She nearly quit when a resident chucked a rock through the dining hall window and facility management had no post-incident meeting to discuss how to prevent or manage those kinds of incidents in the future.
"They had brought this gentleman in and we had no idea what he was about or anything," she said.
The man, she said, didn't know what was wrong or why he did it.
"There's nothing worse than the sound of breaking glass," Severe said.
She wishes she had trusted her instincts to leave.
Severe said there were only two other caregivers and two med-techs with her on any given day. Five of them had to manage about 65 residents, with one caregiver assigned to each unit.
Sometimes she'd radio the others if she needed assistance and she’d get nothing but static.
Every day at about 2 p.m. at Austin House, an employee accompanied residents to the courtyard for a smoke break.
On Jan. 11, 2021, that was Severe’s job.
It was her and about 10 residents, behind a locked gate. She was a little nervous because she'd already been told to “f--k off” that day — by the man who had wrecked the bandage cart. The same man was there, in the courtyard. She watched him pace the perimeter of the fence the whole time.
When Severe told the group it was time to go inside, the man charged her.
He threw her against metal chairs and pushed her to the ground. Then he jumped on top of her, stuck his finger in her eye and "started trying to pull it out," she said.
Severe doesn't know how long she was screaming. But the gate malfunctioned and other employees working that day couldn’t get in to help her until her eye was damaged.
A co-worker pried the man off of her once the gate finally unlocked.
Much of what happened next was a blur. Severe remembers thinking she was going to die. She remembers telling the emergency medical team that she had wet herself and they should put a pad down on the stretcher, to keep it from getting dirty.
She remembers the man shouting, "Die, f--king b---h, die!" as the team carried her off.
Severe said Austin House put her on the schedule a week later. She told them she was never coming back.
The only other communication she got from the place came in the form of a package of frozen chicken noodle soup, delivered to her house a couple of weeks later.
"Not one person called me to see how I was doing," Severe said.
Figuring it out for themselves
Researchers have found that nursing assistants in senior care facilities are more likely to get injured if they're spread too thin.
An employee at Gardens Rehab and Care Center in Kingman got hurt after trying to shower a resident by herself — a resident who was required to have two employees assist him, according to a police report.
When the employee first told the man she needed to shower him, he cursed at her so she went to another co-worker who told her that was just how the man behaved.
She returned to the man's room with backup but her co-worker soon left to bathe a different resident.
Left to shower him alone, the employee turned on the faucet. The man then threw his underwear at her, punched her in the face, threw rags and a soap bottle at her and kicked her in the legs.
The employee told police that no one initially came to her aid when she pulled the call light. Another employee told police they went to help when she walked out of the man's room screaming.
Researchers have found that nursing assistants are more at risk for injury when they're working with dementia or Alzheimer's patients and studies show that dementia-specific training helps.
State law requires that certified nursing assistants receive training that addresses how to respond to resident behaviors associated with cognitive impairment.
In assisted living facilities, managers are supposed to make sure policies and procedures cover how caregivers respond to a resident's "sudden, intense, or out-of-control behavior to prevent harm to the resident or another individual."
But The Republic found only two facilities were cited by the Department of Health Services for failing to do that.
Facilities more commonly get cited for employing caregivers who are unable to prove that they have completed state-mandated training, which includes less than seven hours of instruction addressing resident behaviors related to mental health, dementia or cognitive impairments.
Assisted living managers are required to take 40 hours of classroom training, but fewer than eight hours must be devoted to developing systems for managing residents with dementia, Alzheimer's disease or difficult behaviors.
That's not enough, said Becky Hill, who is on the board that licenses Arizona facility managers and training programs.
"When you're talking about seniors who are extremely fragile, this stuff makes a difference. We're not training people to stock shelves," said Hill. "We're training them to take care of people who have severe disabilities and are at risk every day for falling or choking or having a fight with their roommate."
Meanwhile, turnover is so high at senior living facilities that the training process never stops.
More than 50% of nursing staff left their jobs in half the 122 Arizona nursing homes for which turnover data was available over a one-year period, according to CMS statistics reviewed by The Republic.
There is no equivalent data for assisted living facilities in Arizona. But across the country, the turnover rate for resident assistants at assisted living facilities was 49% in 2022, according to survey data from Hospital & Healthcare Compensation Service's annual Assisted Living Salary and Benefits Report.
Brittani Navarro, who has worked for several assisted living or nursing home companies, said the constant churn of new employees means residents never feel comfortable.
"It takes a lot for residents to trust you to even change them, or to bathe them and then you build that trust and here comes this man that you don't know, and that's a big deal why behaviors go on," she said.
A body to deal with other bodies
After leaving Austin House, Severe needed to find a new job. She could barely see, but she got a position at an assisted living home nearby, juggling shifts with doctor visits and surgeries.
She didn't stay long. She quit because she thought the facility was poorly managed.

Now Severe works four hours a day, four days a week caring for a woman with dementia who lives in her own home. She takes the woman grocery shopping, cleans her house, makes sure she takes her medicine and listens to her stories.
"I don't have anything left (to give) other than companionship," Severe said.
Severe said she will never go back to work for an assisted living facility because she felt so disregarded as an employee and frustrated by poorly trained management and fellow employees.
"People pay major dollars for this kind of care for their loved ones, and then they end up in a facility that doesn’t give a s--t if you live or die," Severe said. "They don't care.
"They just need a body there to deal with the other bodies," she added. "Nobody cares what happens to a person when they can't remember who they are."
Caitlin.Mcglade@arizonarepublic.com, Melina.Walling@azcentral.com, sjayaraman@gannett.com
This article originally appeared on Arizona Republic: Arizona senior living facilities are understaffed, endangering workers

