How 'autoantibodies' could help us understand long COVID and other autoimmune diseases

Antibodies are the specialized fighters that keep your body safe. These proteins produced by the immune system can attach to tiny invaders — viruses or other pathogens — and in many cases prevent them from entering and infecting cells.
Experts talked a lot about antibodies as the COVID-19 pandemic spread: how the proteins reacted to different strains of SARS-CoV-2, to what extent they granted immunity, how long that immunity might last.
But the body produces antibodies against all kinds of outside threats. The question is: what happens when the immune system mistakes part of the body for an outside invader?
The body can create what are known as autoantibodies.
If the body decides to attack itself instead of a pathogen, it can lead to autoimmune diseases or conditions that can cause the body lasting harm. Notorious examples include Type 1 diabetes and rheumatoid arthritis.
But new research from Arizona State University suggests that it’s more complicated than that. Healthy people have autoantibodies, too, and charting their numbers and types may help scientists better understand why they make some people sick.
“The study was basically looking at, ‘do healthy people make antibodies against themselves? And if they do, are they common?’” said Dr. Joshua LaBaer, the executive director of ASU’s Biodesign Institute, whose team conducted the study. “And the answer is they are.”
In a recent meta-review of several previous studies, LaBaer and his team found at least 77 common autoantibodies in healthy individuals. Those autoantibody levels increase throughout youth and adolescence and eventually plateau by adulthood.
He and other scientists have some theories about why those autoantibodies come to be, but they’ll need more research to better understand those mechanisms and why there are differences between different people. If the advances continue, scientists may find better targets for predicting cancers and other supposedly “autoimmune” conditions that may really be linked to prior viral infections.
And that could mean more breakthroughs in understanding long COVID, which we already know is a post-viral syndrome but still a mystery in many ways, including in its diagnosis and in its description.
LaBaer thinks autoantibodies are part of that puzzle.
"Knowing autoantibodies that are common in healthy people would help us identify which are really disease related and which ones are not," LaBaer said.
Latent viruses: He got throat cancer even though he was never a smoker. The cause? An HPV infection
Why the body sometimes produces antibodies against itself
From the moment you’re born, your body starts training to fight against the viruses, bacteria and other microorganisms that proliferate all around us. Immune cells called B-cells pump out specially-shaped proteins called antibodies that can take out specific targets, and other immune cells keep files to help recognize the invaders for future reference.
The immune system, including those antibody-producing B-cells, quickly learns what to attack — and what not to attack — said Ji Qiu, a research professor at the Biodesign Institute.
“Normally we shouldn't produce antibodies against our proteins because (when we are) very young, (like) one and two years old, our immune system was trained to not to mount a response against our own proteins,” he said.
The immune system’s training is strong, but it isn’t perfect. Qiu said its recognition system can be duped.
The body mounts a strong response against infection with a virus, bacteria or fungus, he said, something that has foreign proteins. Those proteins might happen to look a lot like human proteins, and even after the infection is cleared, the body might start to see an enemy when it should be seeing part of the body.
That is why infection with coxsackieviruses (types of viruses related to Hepatitis A and polioviruses) can lead to certain forms of autoimmune diabetes. Those viral proteins look very similar to some proteins in the pancreas, and damage to the pancreas by the immune system can eventually prevent the body from processing glucose normally.
But the proteins LaBaer, Qiu and other ASU researchers found in their meta-analysis, which included nine existing datasets, did not cause disease in their subjects.
Why? Qiu said he has some ideas.
“These proteins (may be) kind of sequestered in immune privileged sites, like in the brain and in the reproductive system,” Qiu said. That means that although those autoantibodies are present in some people, they aren’t hanging out in places where the immune system can easily get to them.
It’s more common to have these autoantibodies than you might think: Qiu said that in their study, he and his team found that as much as 43% of the population might have some of these autoantibodies.
That, he said, was the biggest surprise to him and the most significant finding of the paper in its implications for future research.
Latent viruses: What happens when a virus stays inside you forever?
Biomarkers for disease
The ASU autoantibody study was born from a long-standing interest in finding better ways to detect cancer, LaBaer explained.
“When I'm not doing COVID, my lab is very interested in cancer,” said LaBaer, whose lab has been tracking COVID-19 cases since 2020.
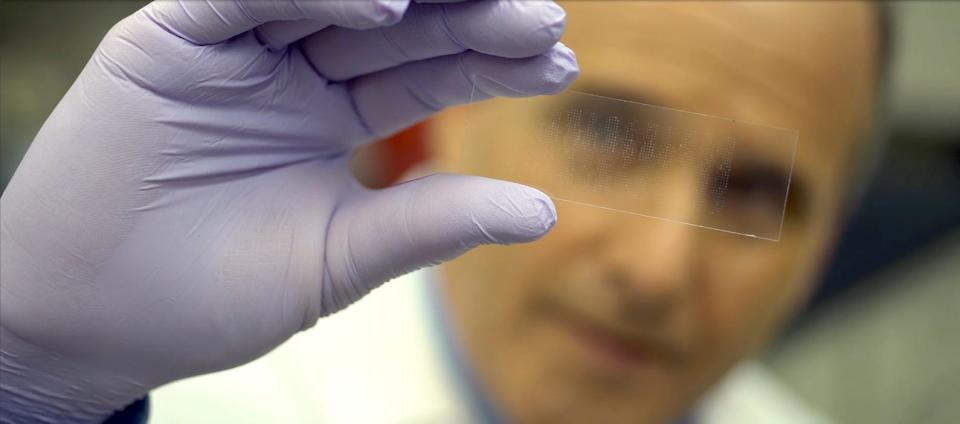
To that end, LaBaer and his team are working on ways to use blood tests to detect antibodies against cancer proteins, an early detection method that can suggest to doctors and researchers that a cancer might be present. It’s one potential application of autoantibodies that LaBaer thinks could be used for many other conditions.
But with the realization that healthy people have autoantibodies comes the task of developing a roadmap of sorts to better use those markers to pinpoint specific diseases.
“These common autoantibodies can confound the search for disease-linked autoantibodies, and their documentation will simplify the identification of autoantibodies specific to certain diseases,” the authors wrote in the article in the journal Cell Reports.
Michael Kuhns, an associate professor of immunobiology at the University of Arizona who was not affiliated with the ASU study, said that having a better handle on what kinds of autoantibodies exist in healthy people may help scientists evaluate "how robust (a particular autoantibody) might be as a biomarker, even a diagnostic.”
It’s just one way that scientists are steadily quantifying and documenting theories that have been in existence for years, theories that draw connections between prior infections and subsequent diseases.
“The idea of a microbial infection leading to antibodies that might cross react with your own proteins is not new," Kuhns said. (By cross react, he means that those antibodies can bind to your own proteins as well as outside ones.) "But having data to support an idea versus just having an idea are two very different things.”
He noted his appreciation for the authors’ decision to list limitations of the study at the end of the paper, which he said was a thoughtful nod to the risks of over-interpreting data.
“They talked about how many samples have statistical power, male versus female and things of that nature,” he said, adding that he thinks it’s important for scientists to recognize the limitations of their experiments and analyses.
“I'm an unabashed basic scientist,” Kuhns said. “I think there's a lot of utility in knowing the basics.”
Long COVID: A virus called EBV, which causes multiple sclerosis, may hold clues
Autoantibodies and the quest to understand long COVID
Qiu thinks those basic principles behind autoantibodies may also be applicable to understanding why some people develop long COVID, the sometimes debilitating collection of symptoms that can set in after a coronavirus infection and range from persistent fatigue to GI symptoms, neurological issues and more.
“Because of the infection, it creates a conducive environment for the immune system to mount an immune response against our self proteins,” Qiu said.
Damage to tissues in the brain, lungs and gut may exacerbate the effects of autoantibody development after a COVID-19 infection, which he thinks might be one of the reasons some people experience symptoms even after the initial virus has passed.
His theory echoes that of Michael VanElzakker, a neuroscience researcher at Massachusetts General Hospital and Harvard Medical School who previously told The Republic how poorly understood “autoimmune” conditions may really be a consequence of the immune system “trying to get at something that was doing damage.”
Understanding that process will take time, as researchers around the world gather data from long COVID patients and sift through the complex array of symptoms they present. That, LaBaer said, is one of the challenges of studying long COVID, because it’s such a new disease that there is still work to be done in defining and diagnosing the condition.
But once they do that and find a sample of patients, “we're going to look to see (if) they make autoantibodies, because we think that they're likely to do that."
For Kuhns, the paper didn’t just present hope of new breakthroughs. It also drove home for him just how complicated a task the immune system has always had in determining whether something in the body is friend or foe.
“We're all teetering on the edge of autoimmunity,” he said. “These kinds of papers give you an idea of the complexity (of the immune system), and how much more we still have to know.”
Independent coverage of bioscience in Arizona is supported by a grant from the Flinn Foundation.
Melina Walling is a bioscience reporter who covers COVID-19, health, technology, agriculture and the environment. You can contact her via email at mwalling@gannett.com or on Twitter @MelinaWalling.
This article originally appeared on Arizona Republic: Why autoantibodies could help us understand long COVID

