Bipartisan State Policymakers Unite To Improve Rural Health Care
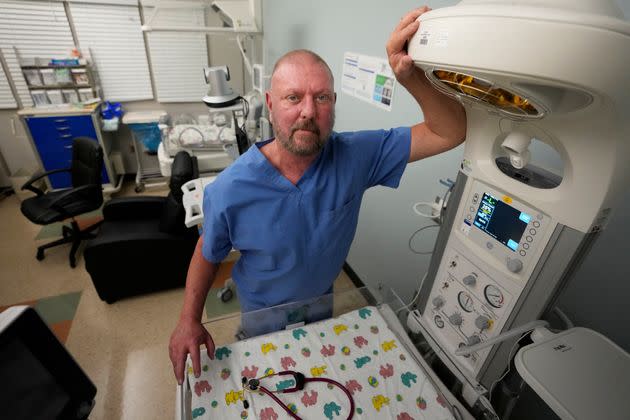
A neonatologist stands in a Paris, Tennessee, hospital's special care nursery that closed this past summer. Tennessee is one of the six heartland states participating in the new caucus.
Health care policy is a partisan lightning rod on the national stage.
But a new, foundation-backed initiative hopes to show that that is not the case among a number of rural states in the middle of the country.
Heartland Forward, a self-described nonpartisan “think and do” tank that emphasizes practical policies for improving life in heartland states and localities, launched the Heartland Health Caucus earlier this month to bring together policymakers from Arkansas, Kansas, Kentucky, Missouri, Oklahoma and Tennessee to discuss solutions to health care problems plaguing rural regions.
The announcement was made at the annual Heartland Summit in Bentonville, Arkansas, on Nov. 8. Bentonville is home to the Walton Family Foundation, the philanthropy of the heirs to the Walmart fortune, which provides some funding for Heartland Forward.
“What’s unique about specifically the Heartland Health Caucus at the state level, across six states, is, No. 1, it’s nonpartisan,” said Angie Cooper, executive vice president of Heartland Forward. “We don’t hear that very often in states across the country.”
Although the six states are mostly dominated by Republicans, Kentucky and Kansas have Democratic governors, and the caucus kickoff confab brought together 19 state lawmakers, policy aides and executive branch officials from both parties. (Two additional officials are participating in the caucus, but could not make it to the Heartland Summit in Bentonville.)
For example, Paula Nickelson, director of the Missouri Department of Health and Senior Services — an appointee of Missouri Gov. Mike Parson (R) — participated alongside Eric Friedlander, Secretary of the Kentucky Cabinet for Health and Family Services — an appointee of Kentucky Gov. Andy Beshear (D).
In consultation with Heartland Forward, the participating states agreed in advance to focus their first meeting on three areas of common interest: health care workforce shortages, maternal health and mental health. At the same time, participants discussed ways that they are using telemedicine and telehealth to tackle all three challenges.
The vibe in meetings between the various officials from each state was upbeat and focused on sharing policy knowledge, according to Cooper.
“I’ve walked into a lot of rooms with policymakers before. Just the energy and the collaboration and the willingness to just roll up their sleeves and say, ‘I need help on workforce shortages,’ or, ’Oklahoma, you just passed a community health worker bill. How did you do that?’”
Expanding Medicaid with federal funds made available under the Affordable Care Act is often seen as an asset for states seeking to shore up distressed rural health care systems. Of the six states that make up the Heartland Health Caucus, four have already expanded Medicaid: Oklahoma, Arkansas, Kentucky and Missouri. Kansas and Tennessee, by contrast, are among the group of 10 states that have refused the expansion money.
Cooper nonetheless said that was not the focus of caucus conversations, which have instead centered on reducing the underlying cost of care.
“The real focus is on that affordability piece,” Cooper said.
Heartland Forward’s convening of the Heartland Health Caucus comes nearly a year after a far-reaching report that the group published last December on the state of health care access in the six heartland states that now form the Heartland Health Caucus.
The report, “Health Care Access in the Heartland,” found that there are major disparities in access to doctors, pharmacists and trauma center hospitals between urban, suburban, and rural counties in those six states. For example, 79.6% of residents of rural counties in those states live in what is known as a “pharmacy desert” — meaning that most residents are more than 15 minutes away from the three nearest pharmacies — compared with 40.7% of the residents of urban counties and 42.2% of suburban counties.
