This brain surgery is a last chance, and there’s only one place in Memphis to get it

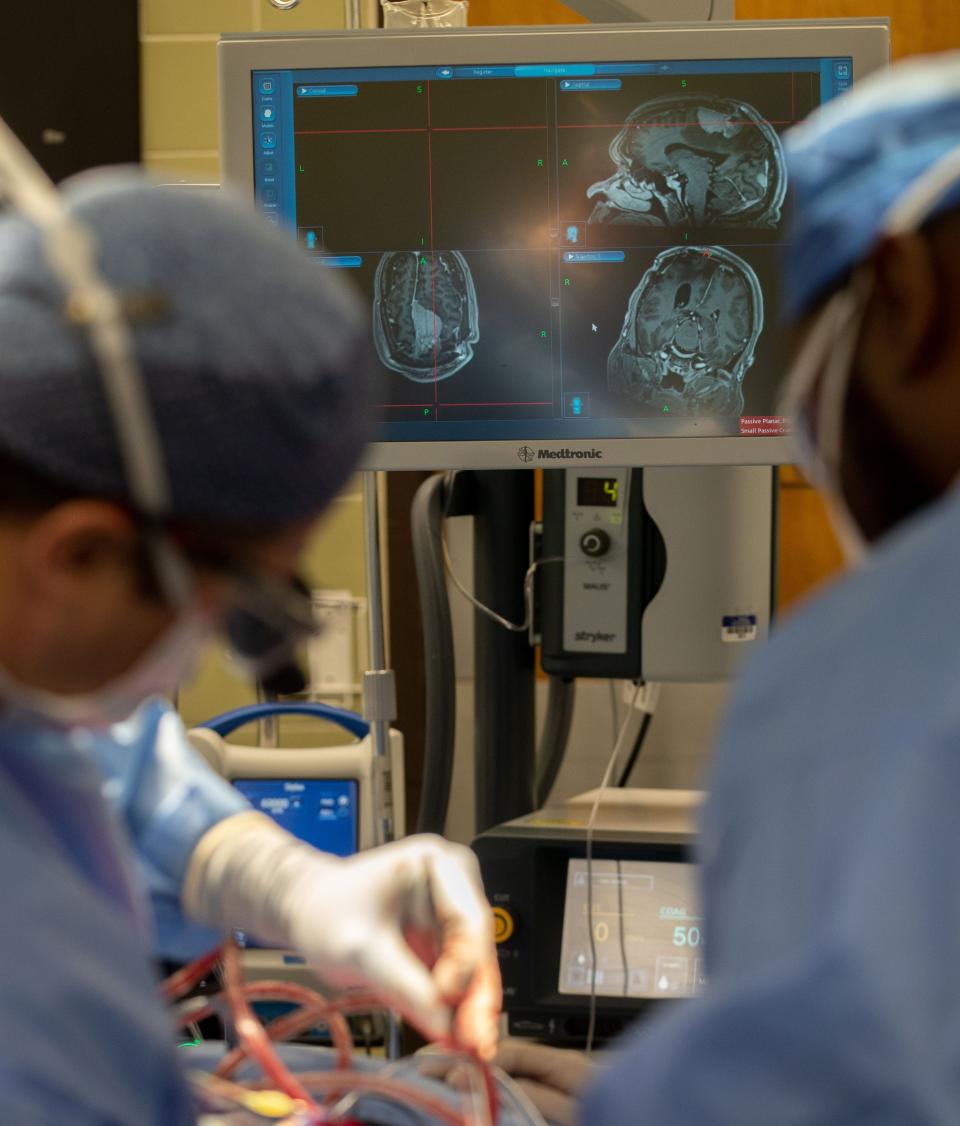
The story below includes graphic photos from a brain surgery at Saint Francis Hospital-Memphis.
Thomas Hunt’s first brain tumor was found on Dec. 28, 2020. He had surgery on Dec. 31, which was followed up by chemotherapy and radiation. However, the tumor “reared its head” in April of this year, his daughter Caroline Greggs said.
Hunt’s oncologist suggested he and his daughter talk to another physician who introduced them to something relatively new, the GammaTile, a tiny device implanted into the brain in a space a tumor used to fill which delivers targeted radiation therapy.
“The whole concept of radiation from the inside out, rather than, you know, outside in was very interesting. And they both said he was a great candidate for it just due to his healthiness otherwise,” Greggs said.

Hunt, 67, had the GammaTile surgery on June 30 at Saint Francis Hospital-Memphis, one of three patients who have undergone the procedure locally. Saint Francis is one of only two hospitals in Tennessee that offer the procedure, according to the company manufacturing the device. TriStar Skyline Medical Center in Nashville is the other.
Greggs said the doctors were able to place the tiles exactly where they wanted to and the surgery had gone successfully. She said she and her father — who has some trouble speaking, which is not uncommon after major neurosurgery — were optimistic after the surgery.
ST. JUDE CHILDREN'S RESEARCH HOSPITAL 'Commitment to Memphis': Here's what St. Jude's $12.9 billion expansion means for the city
HEALTHCARE JOBS IN MEMPHIS: Nurses (and much more) needed: How Memphis hospitals are rebuilding their staffs
Dr. Andy Boucher, a neurosurgeon with Semmes Murphey Clinic, which is partnering with Saint Francis and West Cancer Center to offer the GammaTile surgery locally, and an assistant professor at the University of Tennessee Health Science Center, said for those eligible for the surgery, the alternative generally would be end-of-life care.
“For some of those patients, they would not have another option. It would be palliation or hospice-type discussions. And so this gives them at least another option,” he said.
In a clinical trial, those who received the tile had twice as many tumor-free months compared to their last tumor resection surgery.
The concept is not new. Localized radiation has been utilized for the treatment of other cancers — prostate cancer is a common example, Boucher said — for some time. The difficulty had been finding a way to make it work inside the brain. The GammaTile received approval from the U.S. Food and Drug Administration in 2018.
Placement of the GammaTile — which is under 2 centimeters long — only adds about 20 or 30 minutes to the end of the surgery and recovery for patients is the same as with any craniotomy.
It begins emitting radiation immediately, without having to wait for the surgical wound to heal, and it eliminates any potential negative effects of radiation on other parts of the body.
The radiation is targeted, “cleaning up the edges” of a resected tumor that either could not be entirely removed or where microscopic tumor cells that cannot be seen remain, Boucher said. Healthy brain tissue does not receive radiation from the tile.

It will continue emitting radiation for about 30 days and then the remaining collagen chip is reabsorbed into the brain, negating the need for follow-up surgery to remove the device.
MEMPHIS HOSPITALS: 3 years, 300 babies: How Le Bonheur has saved hundreds of families with 7-minute procedure
ORGAN DONATION: 'The precious gift of life': How 2 Memphis families put power of organ donation on display
In 2020, manufacturer GT Medical secured expanded FDA approval for the tile to be used in the treatment of newly diagnosed tumors. However, Boucher said the GammaTile is generally still used for recurrent, malignant brain tumors.
“We don't have great options for these patients for sort of long-term disease control. So the way we're currently using it in the most common paradigm is that people who have recurrent brain tumors, who often have received radiation before but their tumor still grows back,” he said.
While the tile is not a panacea for brain tumors, it is an important addition to the list of treatments now available for patients with recurrent tumors.
“It's just another tool in the toolbox,” Boucher said. “And it certainly is an option for people, for some of these patients who previously didn't have any more options.”
Corinne S Kennedy covers economic development and healthcare for The Commercial Appeal. She can be reached via email at Corinne.Kennedy@CommercialAppeal.com.
This article originally appeared on Memphis Commercial Appeal: Brain tumor treatment: Memphis hospital offers GammaTile procedure

