Breathing Is Simple. The Way Your Cells Process Oxygen Isn't.
Take a deep breath. In and out.
Simple, right? We breathe all day long without thinking, so it must be a cinch. But for our bodies, and specifically our cells, the process of breathing isn't so easy.
That's the crux of the research from Willima G. Kaelin Jr., Sir Peter J. Ratcliffe, and Gregg L. Semenza, who on Monday morning were awarded the Nobel Prize in Physiology or Medicine. The scientists have spent decades deciphering how our cells use oxygen and adapt to its loss, a condition called hypoxia.
The Nobel Assembly announced the prize this morning at the Karolinska Institute in Sweden. The three scientists will split more than $900,000.
As is tradition, the researchers were unaware of their award before they received the early morning phone call from the prize-granting Nobel committee. “It was so surreal,” Kaelin, a cancer researcher at the Dana Farber Cancer Institute in Boston, said of the early morning phone call in a press conference held by the Institute. “I think I just sort of had this out-of-body feeling of great appreciation.”
Here's why Kaelin and his colleagues earned that early morning call.
Oxygen Is Key
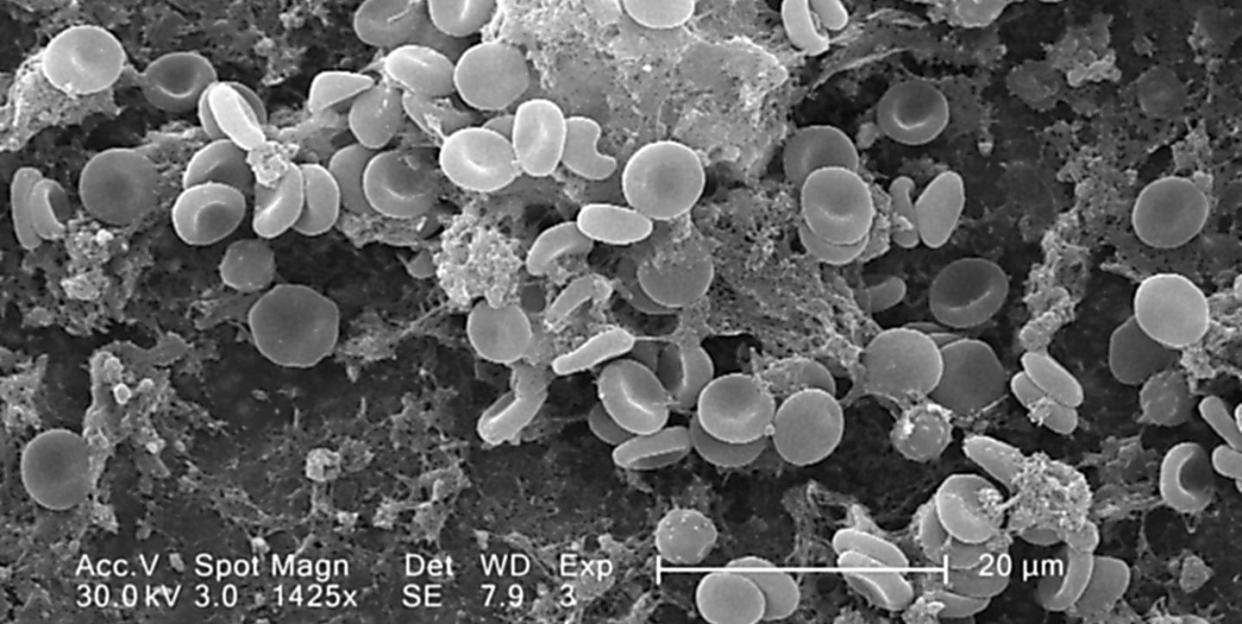
When our cells sense they don’t have enough oxygen, they jump into action by producing a hormone called erythropoietin, spurring the production of blood cells chock full of oxygen-ferrying hemoglobin and creating new blood vessels. Scientists have long understood the relationship between hypoxia and a cell’s ability to create erythropoietin, but they didn’t understand the mechanism behind it: In essence, how do the cells know they’re oxygen-starved?
Kaelin, Ratcliffe, and Semenza began putting the puzzle pieces together.
Throughout the 1990s and 2000s, they identified a molecular pathway that allows cells to sense the amount of oxygen they’re getting. If the cells sense they aren’t getting enough oxygen, they flip on genes that stimulate a response, whether that’s creating more erythropoietin or blood vessels. This work has helped scientists understand the response to hypoxia, which can alter the course of diseases like anemia and kidney cancer.
“It’s sort of a fundamental discovery in the field of cell biology, and it shows that all cells have the ability to respond to changes in oxygen retention,” Emin Maltepe, a neonatologist and developmental biologist at the University of California, San Francisco, tells Popular Mechanics.
Ratcliffe, Semenza, and Kaelin’s research builds on the work of a long line of Nobel Prize winners.
Otto Warburg received the prize in 1931 for discovering the enzymatic process where mitochondria in our cells use oxygen to convert food into energy. In 1938, Nobel Prize-winner Corneille Heymans showed that a person’s respiratory rate is driven by connections between the brain and a cluster of oxygen-sensing cells in the carotid artery. And in 2004, Aaron Ciechanover, Avram Hershko, and Irwin Rose won the Nobel Prize in Chemistry for discovering the proteasome, a cellular machine that regulates the vital HIF protein complex.
A New Hope
Semenza, who works at the Johns Hopkins University School of Medicine, missed the first phone call from Sweden this morning. He wasn’t sure if they were going to call back. “Fortunately, they did,” Semenza said with a laugh at a press conference held by Johns Hopkins.
Both Semenza and Ratcliffe, who is affiliated with the University of Oxford and the Francis Crick Institute, discovered that cells can actually pinpoint when they’re not getting enough oxygen. Semenza is credited with identifying a set of DNA-binding proteins called hypoxia-inducible factor, or HIF, which spur the hypoxia response and activates the genes that make erythropoietin.
Critically, Ratcliffe discovered that cells make these HIF proteins all the time. “If a cell has plenty of oxygen, HIF is always being made and always being destroyed,” Maltepe says. But once the cell goes into hypoxia, production goes into overdrive.
Researchers hope new advances in this field can ultimately develop treatments that help mitigate the effects of hypoxia-related illnesses, such as coronary heart disease and anemia.
People with chronic kidney disease, for example, can't make erythropoietin, and therefore have hypoxic cells, Semenza said. In some parts of the world, a potentially life-saving blood transfusion can fix this, but it can also come with the risk of viral infections, like HIV or hepatitis. Now, erythropoietin can be produced in the lab and injected into patients.
“We have pharmacological tools that can activate this pathway, and can trick the body into thinking you've gone to the top of Mt. Everest,” said Kaelin, also of Harvard University and the Howard Hughes Medical Institute. “There's a series of orally available drugs that are being tested now, where the patient will take the drug, the body thinks it's in high altitude, and starts making more red blood cells.”
An oral treatment for anemia called roxadustat, which prevents the breakdown of HIF and subsequently makes more erythropoietin, is in the middle of a clinical trial in China. Maltepe believes these types of treatments could even be used to treat neurodegenerative diseases or help repair the brain after a stroke.
“There are over 25,000 people in clinical trials for the drugs,” Semenza said. “I suspect that one or more of these drugs may be approved in the next year or so.”
Cancer Co-Opts the Pathway
Kaelin shared a touching tribute to his late wife, Carolyn, an oncology surgeon also with the Dana Farber Cancer Institute, who succumbed to brain cancer in 2015. Kaelin said Carolyn's work and life was a great motivator in his own quest to unravel the complexities our cells’ oxygen response.
Much of his work has focused on a group of proteins related to an inherited genetic disorder called von Hippel-Lindau (VHL) disease. Mutations to the VHL proteins can trick cancer cells into believing they're oxygen-starved.
“What we’ve learned is that when they become hypoxic, they turn on genes that enable them to invade, metastasize, and spread throughout the body,” said Semenza. If the cancer cells create more HIF, they produce more erythropoietin and send blood to the tumors. “We believe it’s these cells that survive the therapy and come back to kill the patient,” he said.
In the case of certain cancers like kidney cancer, Kaelin said, the molecular pathway that regulates oxygen sensing is co-opted.
“They're taking the pathway and they're using it for their own evil purposes,” he said. “Now, because of the work that my fellow awardees and I did, there are other places to intervene with other drugs that will turn the pathway off rather than on.”
Most chemotherapy drugs are currently designed to kill well oxygenated cells, but there’s a dearth of approved treatments that target hypoxic cancer cells. “One of our major goals is to identify drugs that will inhibit HIF activity as an addition to existing cancer therapies,” said Kaelin. “I hope that will help to improve health outcomes in a number of solid cancers."
Together, scientists believe this patchwork of discoveries may help bring us a step closer to shrinking the impact of certain types of cancers.
You Might Also Like

