Britain’s Cherished NHS Wrestles With Its ‘Reform or Die’ Moment
- Oops!Something went wrong.Please try again later.
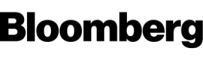
(Bloomberg) -- Britain’s National Health Service has become a story of crisis. A lack of money, a lack of staff, even a lack of beds. The coronavirus pandemic almost broke it - and the hangover still might. This winter has played out against a backdrop of record waiting lists, ambulances unable to deliver patients to hospitals and picket lines of striking nurses.
Most Read from Bloomberg
China Says US Balloons Trespassed Over 10 Times Since Early 2022
US Fighter Jet Downs Fourth Aerial Object Over North America
For a host of medical practitioners and scientists and tech firms and politicians, the NHS – the UK’s biggest employer - has finally reached a tipping point after 75 years, and the time has come to remake it.
Programs and studies underway include “virtual wards” for remote care, family doctors paying energy bills for vulnerable patients and scientists using artificial intelligence to predict the impact of cold and damp homes on children’s health. Their shared focus is finding ways to reduce the burden on the NHS by keeping people out of its overstretched hospitals.
This changing face of the NHS will shift how Britons experience an organization that is ingrained in the national psyche. Data for England show the health service assesses and treats everyone in the country an equivalent ten times a year on average. The shift will hinge on technology and data, making a growing role for private companies – fiercely opposed by some of the service’s staunchest defenders – inevitable.
Britain’s Health Care Black Hole Is Devouring the Whole Country
In normal times, such a shift would be politically impossible. With the next general election less than two years away, though, it’s suddenly on the cards. In part that reflects the scale of the crisis. Yet it’s also because Keir Starmer’s Labour Party, which founded the NHS but has been out of power for 13 years, is surging in opinion polls and appears determined to press the issue.
“If you don't reform the NHS,” Starmer said last month, “I fear it will die.”
Pandemic Legacy
As Covid-19 took hold in March 2020, Watford General Hospital consultants Andrew Barlow and Matthew Knight drew up a blueprint for a “virtual ward” to care for people at home and prevent the hospital being overwhelmed, as was happening in Italy.
More than 6,000 coronavirus patients have since had their pulse, oxygen levels and other data remotely monitored to determine if they need face-to-face care at the hospital north of London, which has also expanded the concept to include people with heart conditions.
“Covid forced us to think differently about how we deliver health care, but this is one of the biggest transformational changes that we're seeing,” said Barlow, divisional director for medicine at West Hertfordshire Hospitals NHS Trust. The next step is to work with patients “at risk of deterioration” so they “don't hit that crisis that brings them to the front door of the hospital.”
Virtual wards are an attempt to solve mismatched capacity and demand, which was exposed brutally by the pandemic. Even before Covid, Britain lagged European peers on key metrics including per-capita hospital beds, critical care and medical technology.
At the same time, cuts to adult social care - support for vulnerable and elderly people at home or in a local facility - created a bottleneck of patients unable to be discharged from hospital wards. That has a knock-on effect, preventing patients being moved from emergency care, which in turn leads to ambulances queuing outside hospitals, leaving seriously ill people waiting hours for callouts.
Lindsey Rutley, a critical care nurse for 25 years, says she spends much of her time now trying to find beds for patients and estimates there are “two or three wards’ worth” at St George's Hospital in south London where she works “who don’t need to be there.”
Rishi Sunak’s Conservative government has embraced virtual wards as a way of meeting a pledge to reduce a backlog for routine NHS care of about 7 million patients. It sees 50,000 people a month being monitored at home to free up hospital space.
Yet critics say potential pitfalls include the risk of “digital exclusion,” if virtual monitoring and appointments become the default. Older people, who may find the technology difficult to use, will also have even less face-to-face contact.
There’s also the question of whether self-care via wearable devices creates demand and data volumes the NHS can’t handle, and whether virtual wards invite more private companies in.
Barlow, who is also chief medical officer at digital care firm Virtue Health, says the argument needs to move on, and that private partnerships are necessary because the NHS can’t create effective software platforms at scale without outside expertise. His West Herts hospital trust is working with medical technology firm Masimo on virtual wards that allow heart failure patients to leave hospital earlier and recover at home.
“You can’t keep throwing personnel at this, it needs to stack up financially – yes you do need consultants and nurses and therapists, but ultimately you have to make it as efficient as possible,’’ he said.
Cold and Sick
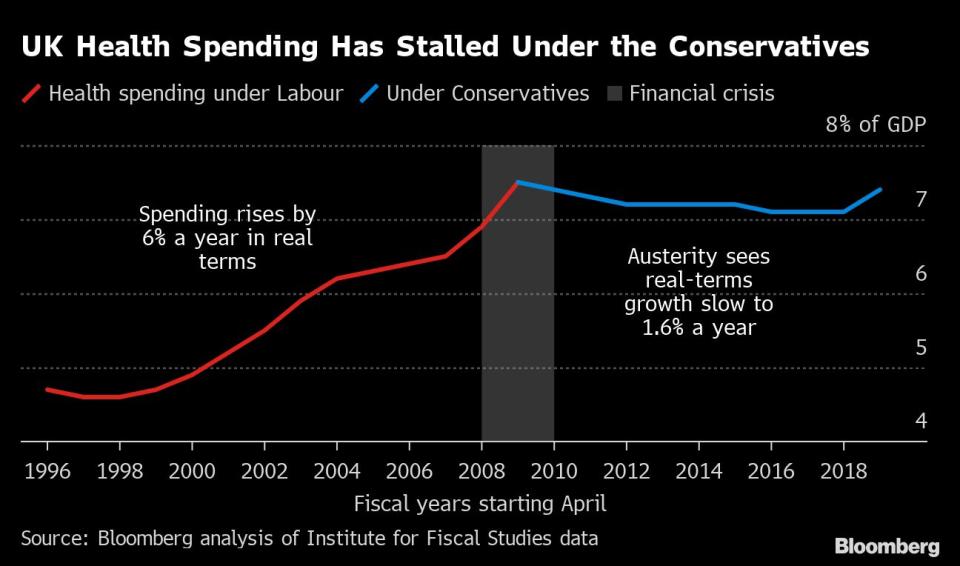
When the NHS started out, life expectancy at birth in England and Wales was 66 years for males and 71 years for females. In the period 2018-2020, it was 79 and 83 respectively – meaning more long-term health conditions, more illnesses that can now be treated that couldn’t before, and of course more elderly care.
That’s a key reason why officials are trying to shift the focus beyond hospitals and treatment to early intervention. The prize is being able to stop conditions from taking hold altogether. “NHS reform on its own is a dead end,” said Richard Sloggett, a former Tory government adviser and founder of think tank Future Health. “What we really need is health care reform.”
In a laboratory at King’s College London, health informatics lecturer Martin Chapman leads a team of scientists using artificial intelligence to “digitally mimic” cold and damp homes and various ways to prevent children living in them from falling ill.
One policy idea they are modelling is a government-funded discount on winter energy bills for low-income households, testing the theory that acting early to prevent chest conditions and mental health problems in young people will save longer-term costs.“It’s like forecasting the weather, except rather than modelling the atmospheric behaviors we're instead modelling human behaviors,” said Chapman, whose three-month study is one of 16 commissioned by the Health Data Research UK charity with funding from the government’s National Institute for Health and Care Research. “The output of our model is a forecast for what will happen, much in the way predicting the weather is.”
Paying energy bills is far from the traditional role of the NHS. Yet research shows it spends an estimated £860 million ($1 billion) treating conditions related to cold homes every year in England, while underheating contributes to about 10,000 UK deaths every winter.
A pilot program in Gloucestershire, southwest England, found tackling the problem at source can help. The study run by tech innovations firm Energy Systems Catapult saw 28 patients prescribed “warmth” in the winter of 2021-22. Recipients reported feeling less stressed about bills and less likely to visit doctors or hospital. A scaled-up trial is running this winter in parts of northeast England and Scotland, funded by energy giant BP Plc.
Going Private
The relationship between the NHS and private sector companies is already a long one: drug makers and tech firms get access to a pool of patients and the health service gets the latest developments. Businesses provide extra capacity in hospitals for surgery and beds, and most family doctors - known as general practitioners or GPs - operate in private partnerships.
But it still leads to the accusation, especially on the political left, that firms are driving up costs in a taxpayer-funded service. An NHS project to unify patient and other data, regarded as critical to coordinating care and managing resources, is providing the latest flashpoint.
The frontrunner for the £480 million contract is Palantir Technologies Inc., a US software and consulting company co-founded by Peter Thiel. He described Britons’ affection for the NHS as “Stockholm Syndrome” last month and said the service – which “makes people sick” - needs “market mechanisms” including privatization and deregulation to fix.
Thiel Scorns Britons’ Embrace of NHS as Palantir Seeks Contract
Palantir, which said Thiel had been speaking as a private individual at the event in Oxford, got its foot in the UK’s public health door during the pandemic, offering its Foundry software to manage the Covid-19 vaccine rollout for just £1.
Several vendors and NHS officials told Bloomberg that rivals for the data contract would find it difficult to unseat Palantir, now its software is embedded in the health service. Others that have expressed an interest include C3 AI, an enterprise artificial intelligence software company, and British data analytics firm Quantexa. The NHS has yet to announce the successful bidder.
Palantir’s involvement with the NHS sits uneasily with civil liberties groups given its tools have been used by US Immigration and Customs Enforcement to find undocumented migrants, for example. Patient advocacy group MedConfidential argues the health service should build its own open-source platform, rather than tie itself to Palantir.
But the trend of private companies eyeing parts of the NHS shows no sign of slowing, with the post-pandemic crisis and patient backlog creating more opportunities.
Gresham House Ventures, which in 2020 invested £5 million in eConsult Health - an online consultation form used by more than 3,200 GP practices – sees remote monitoring as a key area for growth.
“If you look at the causes of the waiting list, it’s not the access to treatment,’’ Gresham House’s investment director Maya Ward said. “It’s actually the diagnostics to identify the optimal treatment.”
Even the Labour Party, with its ties to health unions traditionally wary of the link between modernization and private companies, seems relaxed about their involvement. It has said private hospitals could be handling 230,000 extra operations a year to cut existing NHS waiting lists.
Tipping Point
Amid the post-pandemic turmoil, public satisfaction with NHS service levels is falling. As of November, close to 380,000 patients had been waiting more than a year for treatment, such as general surgery, neurology and cardiology. The delay is keeping people out of the workforce.
It’s also pushing more people to opt for private health care – about one in eight adults did so in 2022, with more than half self-funding on a pay-as-you-go basis rather than via insurance. Cataract surgery, hip and knee replacements and hernia repair procedures saw big rises, according to the Private Healthcare Information Network, an independent researcher.
Lack of access to NHS GPs has driven a rise in private app- or web-based services. Before the pandemic, AXA Health’s virtual GP service was handling about 4,000 appointments a month; it’s now more than 50,000, commercial director Fergus Craig said in an interview.Staff are also leaving in part to seek better pay and conditions in the private sector. According to NHS England, the service had a nurse vacancy rate of 11.9% or 47,496 unfilled positions as of September.
There’s Never Been a Worse Time to Get Sick in the UK
The cost of funding the NHS keeps rising. The government spent £184 billion on health and social care in the year ended March 2022, of which NHS England accounted for about £150 billion. Getting waiting lists down and making improvements will likely require much larger sums to be spent.
There appears little appetite among the British public for free health care to be watered down. It’s why neither Labour nor the government are talking about changing how it is funded – though Sunak has suggested people should pay if they miss an NHS appointment, an idea he abandoned after becoming prime minister.
“What we've seen in the past is when NHS waiting times start to fall, you see the interest in self-pay completely go,” said Sally Warren, director of policy at the King's Fund health think tank. She expects the current trend to reverse – so long as the NHS can get back on track.
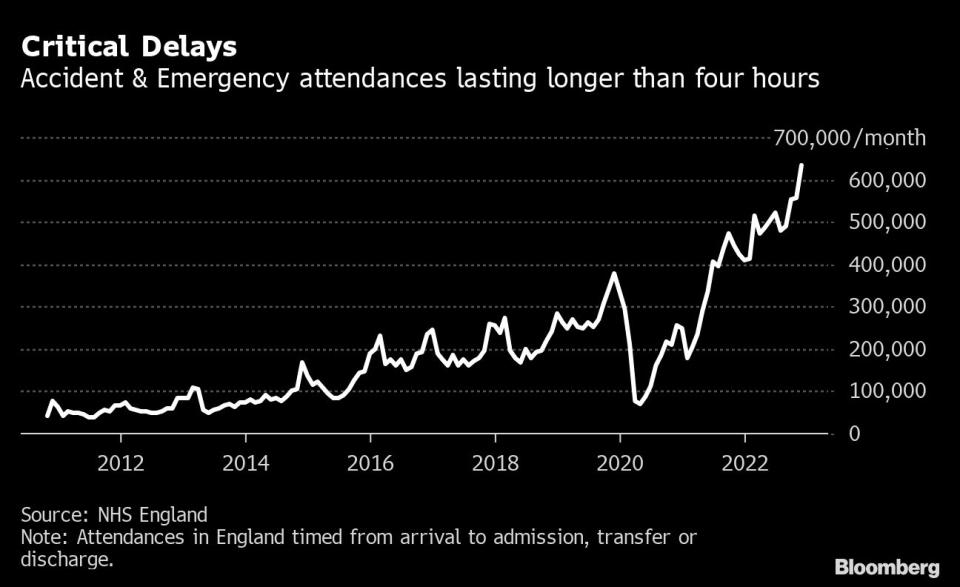
That's not easy after funding for both social care and public health programs were slashed in the decade following the 2008 financial crisis.
Warren, who used to work for the government on social care policy, said ministers have been talking for 20 years about shifting care out of hospital: “All the politicians say it, but yet they're unable to lead a system to make those changes."
Labour Push
Part of the problem is an electoral cycle of about five years, which makes governments wary of long-term plans and puts a premium on wooing voters with new hospitals.
While Sunak has embraced the idea of virtual wards, he has been more cautious about a broader overhaul. The legacy of austerity and previous unpopular reforms have left the Conservative government tainted, and even some Tory ministers privately concede it’s Labour that has the credibility with voters to talk about fundamental change.
Embracing a rethink is not risk-free for Labour, even as polls put it on course for a comfortable election victory, and Starmer faces considerable pushback from party members if he yields too much ground to private firms.
Labour is promising a 10-year-plan – effectively two terms of government - to modernize health care. Starmer has said that stems from his experience as director of public prosecutions, when it was rare he came across a case that couldn't have been prevented earlier in life.
Back on the picket line outside St George's Hospital, critical care nurse Natasha Trenchard-Turner said it’s now or never for an NHS she has worked for since 2002.
“I want to be hopeful,” she said. “You need a consistent plan that has evidence behind it, they need to commit to it and they need to fund it. And that's the only way we're going to save our NHS.”
--With assistance from Olivia Solon, Irina Anghel, Eamon Akil Farhat, Katie Linsell and Andrew Atkinson.
Most Read from Bloomberg Businessweek
©2023 Bloomberg L.P.