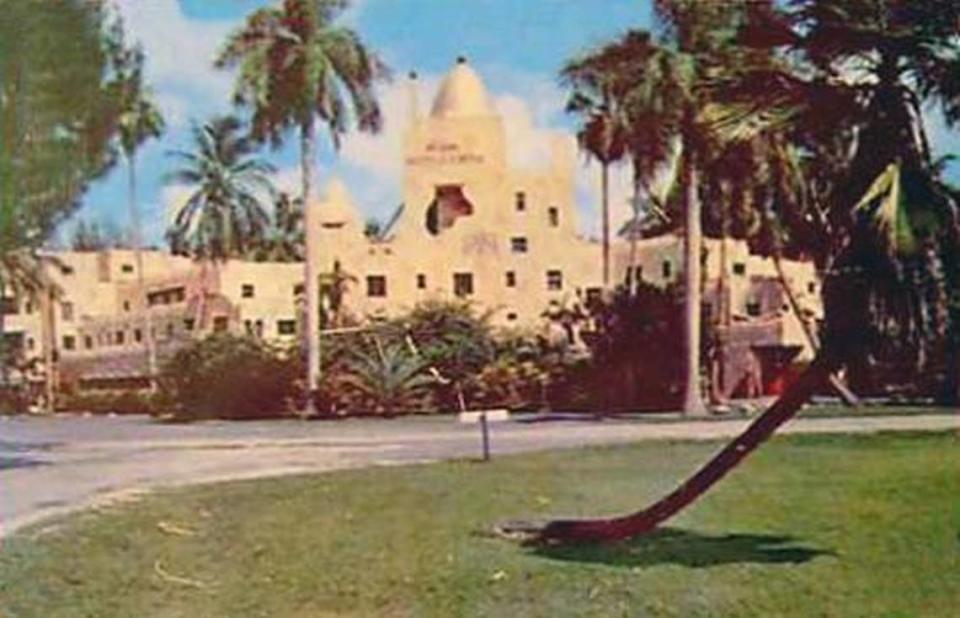
At Miami Springs nursing home with slew of deaths, state cited sloppy anti-COVID procedures
The Fair Havens Center Nursing Home in Miami Springs reported 14 additional COVID-19 deaths in the past week, bringing the total number of resident fatalities at the home to 22. It’s the most in South Florida and second most of any long-term care facility in the state, according to data released Friday by the Florida Department of Health.
Earlier in the week, the state halted new admissions to the nursing home, citing ineffective COVID-19 monitoring and isolation practices that created a “fertile ground for the virus to spread.”
Florida nursing homes and assisted living facilities (ALFs) accounted for nearly three out of every four COVID-19 deaths in the state in that one-week span, the latest statistics from the DOH indicated.
One Florida home has had more deaths than Fair Havens — Seminole Pavilion in Pinellas County, which has tallied 25, including one staffer.
Among other homes near the top of the list for COVID-19 deaths, Manor Pines in Broward has had 17 and one in Miami-Dade, Claridge House, has logged 14.
Overall, the 844 deaths associated with nursing home and ALF residents and staff members have accounted for 44% of the state’s 1,917 COVID-19 deaths to date. Facilities in South Florida, the hardest hit area in the state, have accounted for nearly half of the COVID-19 deaths at long-term care facilities across the state.
Still, there were fewer deaths this past week at nursing homes and ALFs than in the previous week, as the state tries to ramp up testing in long-term care facilities and continues to institute restrictions designed to prevent positive COVID-19 patients from being transferred from hospitals to nursing homes as elders move back and forth.
Gov. Ron DeSantis has, however, balked at recommendations by the White House coronavirus task force for states to mandate testing at all elder-care facilities, leaving it up to individual homes.
The state has created “strike teams” of National Guard medics to come into facilities that request testing, but the Herald previously reported that these teams had tested fewer than 6% of the state’s homes as of earlier this week.
Just what is occurring inside Florida’s 700 nursing homes and 3,100 assisted living facilities is a bit of a mystery. The Herald’s tip line has been flooded with complaints from family members who cannot see their loved ones because of a protective lockdown but are also struggling to learn in real time whether residents and/or staffers have contracted the coronavirus and how many, if any, have died.
Only under the threat of media lawsuits did Florida begin publicizing information about individual nursing homes, first just a list of places that had COVID-19 cases but not differentiated between staff and residents and with no death totals. Weeks later, the state began providing a broader data set, now released on a Friday night schedule, that provides some glimpse of the facilities worst hit by outbreaks.
But there is scant detail.
The state’s emergency order halting new admissions to Fair Haven said that instead of isolating residents who had been exposed to COVID-19, the facility transferred 11 former roommates of COVID-19 positive residents to two-bedrooms with other residents who did not have coronavirus. And the home’s nursing director indicated that the facility did not isolate residents with known exposure to COVID-19 if the resident had not yet been tested.
The agency also observed a wound-care nurse in the home’s COVID-19 unit reusing protective gear after visiting a positive resident, merely washing her hands and changing her gloves. An occupational therapist feeding a resident in the COVID-19 unit wore only a surgical mask and gloves rather than full protective gear.
A story published Thursday in the Herald documented how a Panhandle nursing home in Calhoun County — Blountstown Health and Rehabilitation Center — was also hit with a moratorium on new residents. In that story, the influential seniors’ advocacy group AARP weighed in with a startling statistic: 80 percent of the 48 coronavirus deaths reported Wednesday night into Thursday were elder-care deaths.
“When one-fiftieth of the population is suffering four-fifths of the deaths the need for action could scarcely be clearer,” Jeff Johnson, Florida director for the AARP, said in a statement to the Herald.
With information lacking, the Herald has used proxies to gauge what is happening. No one answered the phones at the Fair Havens Center Friday, but a log of 911 call records from the Miami Springs Police Department shows that there were 14 responses to Fair Havens between March 27 and May 13 that specifically cited COVID-19 as the nature of the emergency.
Before that, from Jan. 1 to March 27, the call logs show there were seven persons reported dead on arrival at the address for Fair Havens, and 24 calls involving a sick or injured person. It’s unclear how many of those, if any, were COVID-19 related.
National eyes, local problem
What happens in the state’s nursing homes is being followed across the nation, in part because Florida has long been the leading retirement destination, where seniors from across the country spend their twilight years.
President Donald Trump hosted DeSantis at the White House on April 28, where the Florida governor touted the state’s infection numbers as lower than some other states, particularly in the Northeast. This past week, in the same setting, coronavirus task force member Dr. Deborah Birx suggested that all residents and staffers at elder-care facilities be tested over a two-week period regardless of whether they show symptoms.
A recent Herald story spotlighted the difficulty some nursing home operators said they faced in getting widespread testing. And a story this week detailed DeSantis’ opposition to the state taking responsibility for testing all elder-care residents.
It wasn’t the only time nursing homes became the topic of White House discussion. At a May 8 meeting between Trump and GOP lawmakers at the White House, Pennsylvania Rep. Guy Reschenthaler criticized his state’s Democratic governor, businessman Tom Wolf, for issuing a blanket stay-at-home order instead of “protecting the most vulnerable in nursing homes, where you had 65 percent of the deaths, if not more, in Pennsylvania.”
COVID-19 Cases in Florida
Federal and state public health officials have warned against a hasty lifting of protective health orders, in part because the elderly are so much more vulnerable to a respiratory virus that can pass through people who have it but do not show symptoms.

