Is my child going to lose Medicaid? What families need to do now to avoid being dropped
For three years after the pandemic began, people who have Medicaid health coverage were automatically reenrolled, and didn't have to verify annually that they qualified for this benefit.
That continuous Medicaid coverage ended on March 31. In Texas, the end to continuous coverage means that the state has to reverify that 2.7 million women and children still qualify for Medicaid to keep them enrolled.
The U.S. Department of Health and Human Services predicts that as many as 15 million people nationwide could be disenrolled in Medicaid during this process, including 6.8 million who still qualify for Medicaid.

Why is the end of continuous Medicaid coverage important?
Staff at local clinics worry that families might not be aware of the changes, said Lucy Sumner, vice president of revenue cycle at Austin Regional Clinic. These families are working to make ends meet, caring for children, lacking time to work through red tape on the phone or on the computer, or might have moved.
Clinics worry that if families don't maintain their Medicaid status, they might put off preventative care, which many kids fell behind on during the pandemic. Families also might seek nonemergency care at the emergency room rather than go to a primary doctor because they can't afford health care.
Who can get Medicaid?
Medicaid qualifications are based on family size and monthly income. For example:
A family of four making less than $3,083 a month qualifies for Medicaid for their children.
Some parents in extreme poverty can get Medicaid if a family of four, with two parents, earns less than $285 monthly.
Families with children with disabilities can qualify if they cannot afford health care premiums.
Pregnant women with a family of four making less than $4,579 a month can receive Medicaid during pregnancy and up to two months after the baby's birth. There are bills in this Texas Legislature this session to extend it to a year.
Learn more: Texans can be at risk for Medicare fraud. What you need to know to protect yourself.
What do I need to do?
Starting this month, you have to verify your income and make sure Medicaid has your current contact information to stay enrolled.
Create or log into your account at YourTexasBenefits.com or the Your Texas Benefits app. In your account, ensure your information is correct, including address, phone number, email, family size, age of children and income.
You can call 211 and press option 2 or go to your local Medicaid enrollment office. To find a Texas Health and Human Services office or a community partner, visit yourtexasbenefits.com/Screener/FindanOffice.
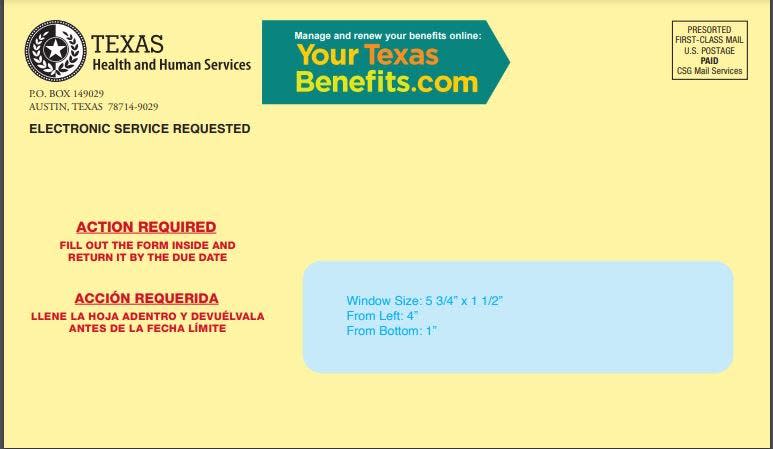
Then watch your mail or email. Yellow envelopes with red lettering that say "Action Required" are being mailed to people with a renewal form. If you have a YourTexasBenefits.com account, that form will come electronically.
Once you have the form, you need to return it by the due date, in some cases in 30 days. You need documentation to verify your income and identity. You can submit the application, renewal form and information by:
Mailing to Texas Health & Human Services, P.O. Box 149024, Austin, TX 78714-9024
Faxing to 877-447-2839
Calling 211 and choosing option 2 after picking a language.
Visiting a local office or a community partner.
What happens if I don't turn in my renewal packet or request for information?
Benefits will be terminated. You will receive a notice stating that you will no longer receive health care coverage. You will have 90 days to respond, and the state will process your information without requiring you to submit a new application. After 90 days, you have to fill out a new application.
What is the timing of the reenrollment?
Texas began sending out letters about reenrollment in January.
The actual re-verification process continues throughout the year. The first renewal applications went out April 8. Batches of applications will be sent through September. The state is prioritizing reenrollment of people most likely to no longer qualify first. These are:
People who have turned 19 during this three-year period.
Previously pregnant women who had their babies and are past the postpartum period of coverage.
People known to have had a change in family income.
Then the state will start working through the remaining 2.7 million women and children who receive Medicaid.
The re-verification process is not likely to affect Medicaid programs for seniors or people with disabilities.
Access to care: Central Health's demographics report: a story of poverty and health access in Travis County
What happens if my family no longer qualifies for Medicaid?
If children qualify for the Children's Health Insurance Program, or CHIP, which allows for a higher family income, the state says it would enroll kids in CHIP. Families who still don't qualify will be given information about other resources, including the insurance marketplace on healthcare.gov.
Families also can go for care to federally qualified health clinics such as CommUnityCare, People's Community Clinic and Lone Star Circle of Care, which offer sliding-scale fees based on income.
If my child loses Medicaid, can we still get treatment?
Losing your health insurance doesn't mean you do not have care, said Lone Star Circle of Care’s Chief Operations Officer Lindsey Tippit. For emergencies, safety-net hospitals will treat patients regardless of their health insurance status.
"If you go to our hospital, our ER, we're going to make sure we take care of you no matter what," said Geronimo Rodriguez, chief advocacy officer at Ascension Texas, which includes Dell Children's Medical Center and Dell Seton Medical Center, the safety-net hospitals for children and adults in Travis County.
If a child who should qualify for Medicaid and doesn't have it arrives at the hospital, staff at Dell Children's will direct parents on how to enroll. Until they are enrolled, families might have to pay out-of-pocket for care, though Dell Children's and Ascension Texas have charity care funding.
If families are de-enrolled in Medicaid, they can go to doctors' offices that are not federally qualified health clinics, but pay out of pocket for the visits until they can get reenrolled. ARC's Sumner expects this will have a "massive" impact on patients, and "there's going to be a lot of unanticipated bills."
Does this affect other benefits such as SNAP, TANF and CHIP?
No. Those federal programs are not affected by the end of continuous Medicaid coverage.
How else is the state trying to reach people?
Texas Health and Human Services has been using social media posts, handing out flyers in community settings and sending Medicaid participants emails and texts to alert them of the changes. It also has an FAQ online to help answer questions.
What are clinics and hospitals doing to help people keep their benefits?
Clinics and hospitals across Central Texas are working to identify and reenroll their Medicaid patients.
At Dell Children's clinics and hospitals, staff have resource cards to help families. Austin Regional Clinic mailed 30,000 letters to patients on Medicaid about the reenrollment process. At Lone Star Circle of Care, where 45% of its 97,000 patients are on Medicaid, the patient services team is ready to help patients stay enrolled.
"We're trying to make this as smooth as possible," Tippit said. "Families don't have to navigate this alone."
This article originally appeared on Austin American-Statesman: Here's what Texans need to do to avoid losing Medicaid coverage

