Children’s mental health issues have increased, insurance claims suggest
Story at a glance
Childrens’ mental and behavioral health have suffered during the pandemic.
A new report looks at insurance claims data from 2016 to 2021.
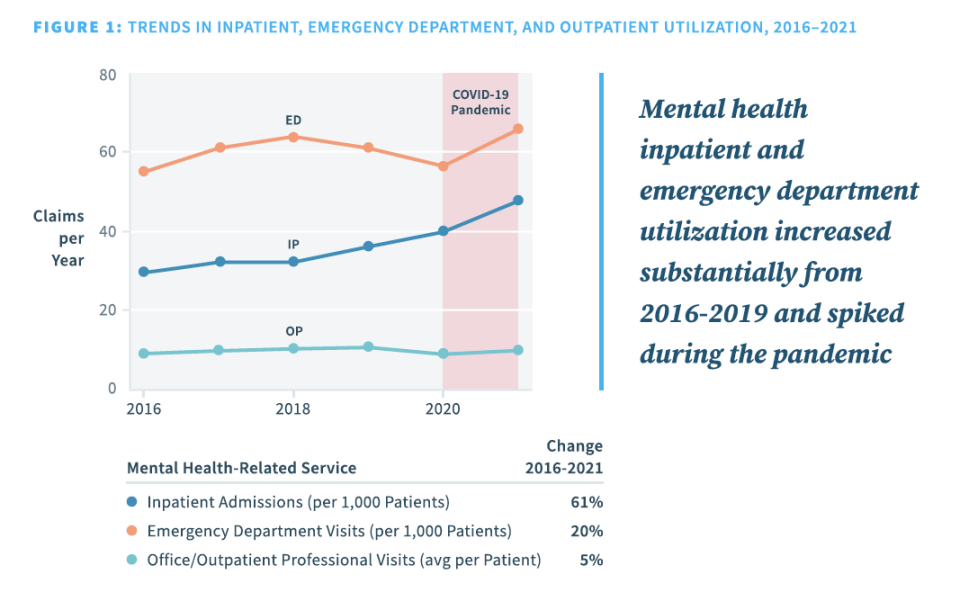
There was a 61 percent increase in mental health related inpatient admissions and 20 percent increase in emergency department visits.
Mental health in children and teenagers has suffered during the coronavirus pandemic. The U.S. surgeon general issued an advisory at the end of 2021 warning about a mental health crisis in youth, and a 2020 report from the Centers for Disease Control and Prevention suggested that mental health related emergency department visits in children started increasing in April of that year and stayed high through October.
A new report from Clarify Health Institute, the research arm of payments platform company Clarify Health, breaks down the data covering 2016 through 2021 for mental health related insurance claims for children ages 1 to 19. Overall, there were increases in most claims related to mental health, sometimes very sharp increases starting in 2020.
The data includes claims for about 20 million children annually from 2016 through 2021, approximately covering the first two years of the coronavirus pandemic. The records include inpatient admissions as well as emergency department visits and outpatient/office professional visits. Inpatient admissions typically mean that the patient needs to stay overnight, whereas for outpatient visits they do not.
Overall, there was a 61 percent increase in mental health inpatient admissions, from 30 to 48 visits annually per 1,000 patients. There was a 20 percent increase in emergency department (ED) visits, from 55 to 66 visits annually per 1,000 patients.
Some of the mental and behavioral health conditions in the analysis include depressive disorders, other mood disorders, anxiety disorders, stress disorders, feeding and eating disorders and suicidal ideation.
By age groups, teenagers aged 12 to 15 and 16 to 19 fared worse than the younger age groups. Girls aged 12 to 15 had an 84 percent increase for inpatient admissions per 1,000 patients, and boys in the same age group saw an 83 percent increase. ED visits increased by 41 percent for girls and 38 percent for boys in this age group.
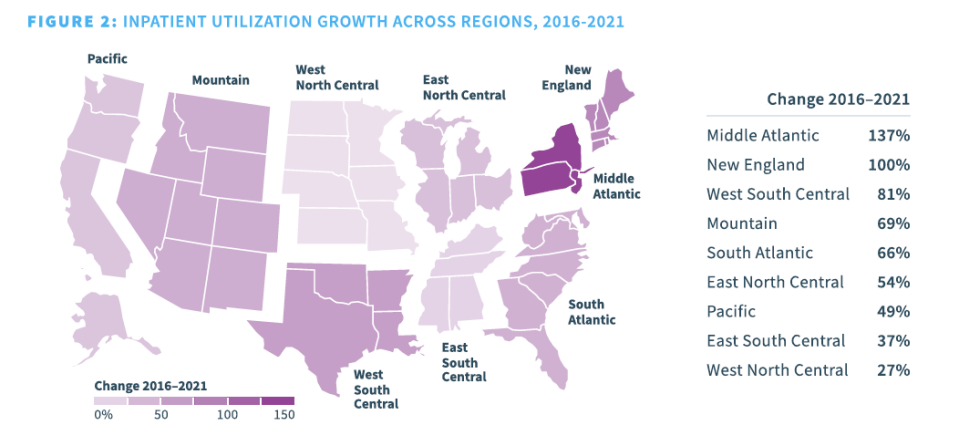
The report authors also laid the data out by region. The middle Atlantic region saw the largest increase of 137 percent more inpatient utilization of mental health services. The next highest was New England (100 percent increase), followed by West South Central (81 percent increase; which includes Texas, Oklahoma, Arkansas and Louisiana).
Comparing commercial insurance users to Medicaid users, claims to commercial insurance increased more rapidly than for Medicaid. Historically, inpatient mental health claims in children are higher in Medicaid users, but in 2021 the inpatient usage in the commercial insurance population surpassed Medicaid.
“The trends illuminated in this report reinforce healthcare leaders’ responsibility to address children’s mental health, especially when considering that half of all mental health conditions onset during adolescence and carry into adulthood,” said Jean Drouin CEO and Co-Founder of Clarify Health, in a press release. “With a growing consensus that mental, behavioral and physical health intersect, this research report aims to spark a conversation about the overall wellbeing of America’s next generation.”
For the latest news, weather, sports, and streaming video, head to The Hill.

