COVID takes a back seat: Here are the 2023 health threats getting all the buzz in Florida
Florida has seen multiple scares surrounding diseases since the beginning of the year which may grab the attention of people concerned with their health and potential risks. Leprosy, the rare disease which mostly affects the skin and peripheral nerves, may possibly even become endemic in the southeastern U.S. according to the Centers for Disease Control and Prevention (CDC).
The Florida Department of Health (FDOH) has been providing updates on the incidents in collaboration with the CDC in order to keep Floridians and travelers aware of potential health risks.
As COVID-19 takes a backseat to the imminent worries surrounding these diseases, here are some things that Florida residents and visitors may want to know about them.
Leprosy in Florida: Leprosy could become endemic to Florida. Here is what to know.
Are COVID cases going down in Florida?
Data from FDOH reveals that there were 9,942 COVID-19 cases in Florida as of the week of July 14. The number of cases in the state had surged in the 10 weeks between May 12 and July 14, initially starting at 5,607 cases on May 12.
Researchers point out that the number of reported new cases is likely lower than reality as more and more people with symptoms use at-home rapid tests and do not report the results to state and federal health authorities. Meanwhile, new case positivity rates in Florida have more than doubled in the past 10 weeks, going from 7.7% on May 12 to 17.4% on July 14.
FDOH has recorded more than eight million Floridians who have completed their series of vaccinations against COVID-19 thus far and nearly six million who have received at least one additional/booster dose.
Why is leprosy on the rise in Florida?
Rising numbers of leprosy cases in the southeastern U.S. has led the CDC to suggest in a new research letter that leprosy may soon become endemic in the region, with many of the cases coming from Central Florida. In their "Emerging Infectious Diseases journal," they state that Central Florida accounts for 81 percent of cases in the region and nearly a fifth of the entire nation's.
The means of transmission for the disease, also know as Hansen's disease, within the region has not yet been explained, warranting further research into other methods of local transmission. Many of the recent cases from Central Florida lack the traditional risk factors associated with leprosy which, when combined with the high proportion of residents, supports an investigation into environmental reservoirs as a potential source of transmission.

Leprosy, otherwise known as Hansen's disease, is a chronic infectious disease that primarily affects the skin and peripheral nerves in the body and is caused by Mycobacterium leprae. The disease has been traced to as far back as 600 B.C. with incidents in China and India.
Leprosy has historically been an uncommon development in the U.S. Incidence peaked in 1983 and drastically reduced year-by-year until 2000. Over the past decade, the number of cases has doubled in the southeastern region of the U.S. despite 95 percent of the world's population having a natural-born immunity to the M. leprae bacillus.
Modern leprosy is treatable and curable.
Early diagnosis and treatment usually prevent disabilities that can result from the disease, and people with Hansen’s disease can work and lead an active life. Once treatment is started, the person is no longer contagious. However, it is very important to finish the entire course of treatment.
Is malaria common in Florida?
Seven cases of the disease Malaria have been confirmed in Sarasota County. This is the first local spread that the region has seen in two decades after eight cases were confirmed in Palm Beach County in 2003. According to the CDC, these seven patients infected by malaria were promptly treated at area hospitals and are recovering.
The CDC has been collaborating with FDOH on the seven locally acquired cases of Plasmodium vivax malaria in Sarasota County. Typically, malaria cases in the U.S. are imported by people who travel to countries where malaria is endemic, but locally acquired mosquito-transmitted malaria cases are still possible.
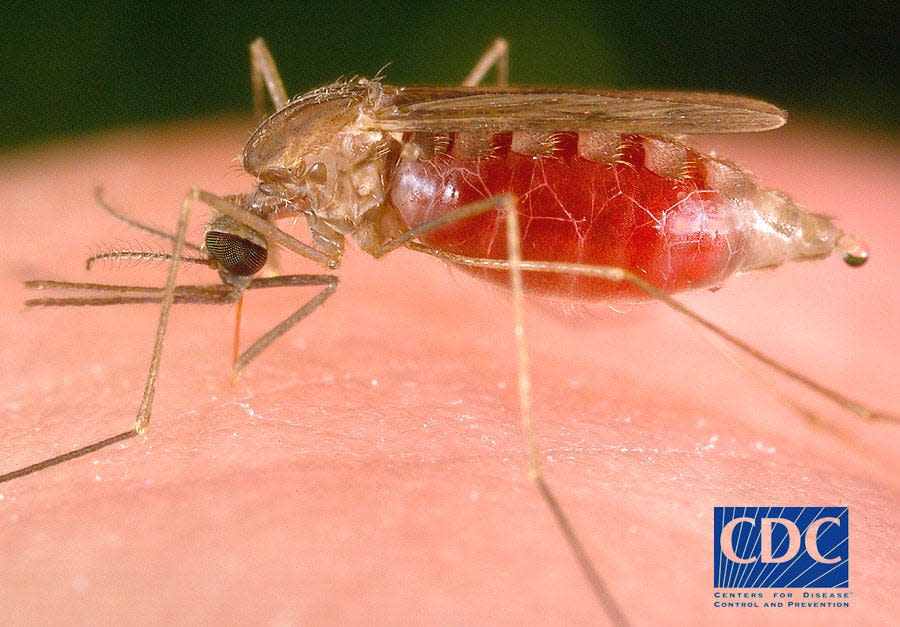
FDOH is also working with local partners and county mosquito control in Sarasota County and Manatee County in order to prevent further transmission of malaria and enhance case detection.
The CDC issued a public health alert in June advising doctors, public health authorities and the public about the risk and what to look for. "Despite these cases," the letter said, "the risk of locally acquired malaria remains extremely low in the United States."
Malaria is a mosquito-borne disease caused by a parasite. A bite from a female Anopheles mosquito will infect an individual and leave them with symptoms like fever, chills and flu-like illness. An untreated malaria infection can leave a person with anemia, jaundice, kidney failures and worse.
What are brain-eating amoeba?
An person in Charlotte County died in March after being infected by the brain-eating amoeba Naegleria fowleri, which can infect people when water containing it enters the body through the nose. FDOH in Charlotte County suggested that the infection could have been a result of doing sinus rinse practices with tap water.
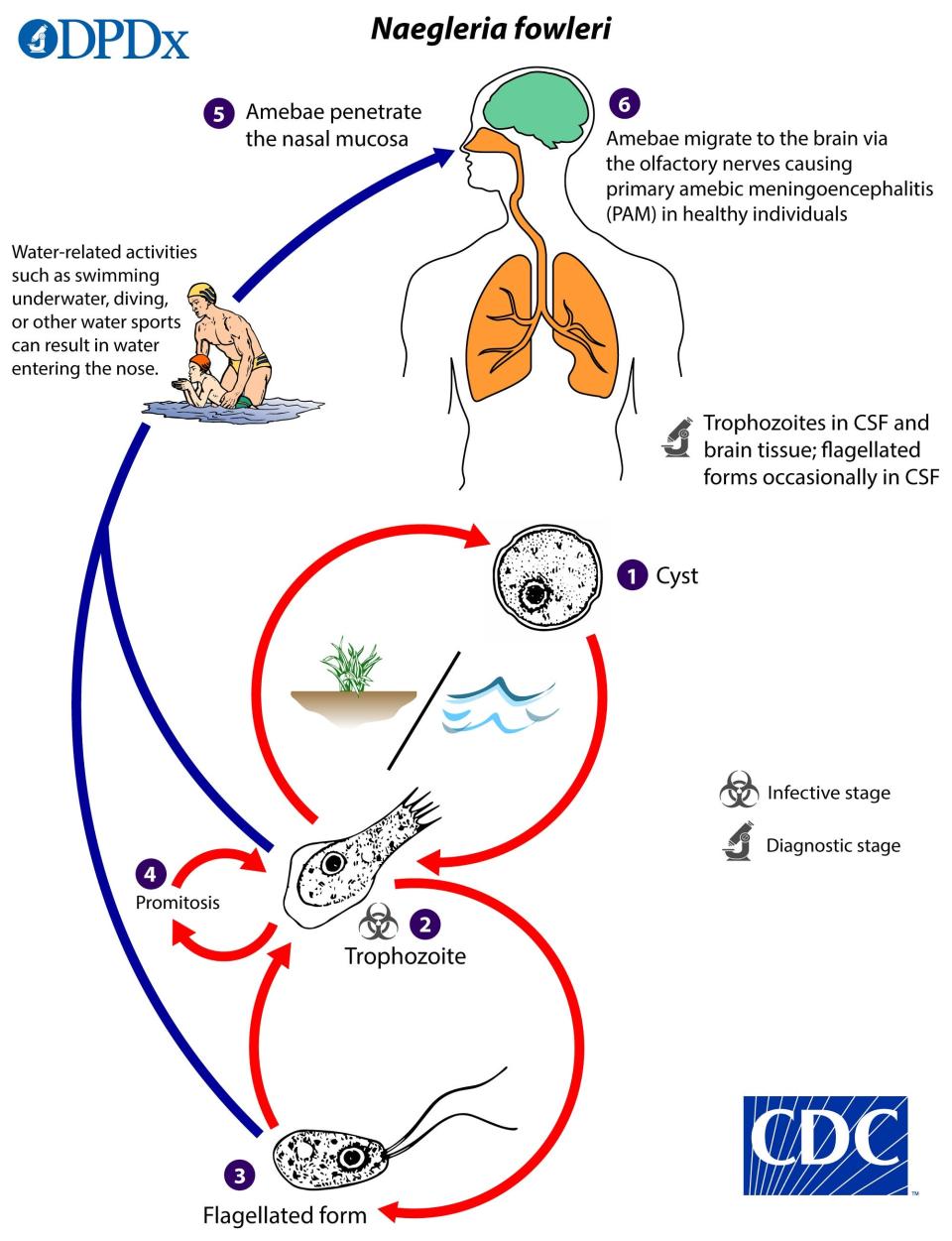
A 14-year-old boy from the same county miraculously survived after being infected by the amoeba last July, which has a fatality rate of 97 percent.
Naegleria fowleri is a microscopic, single-celled ameba that is commonly found in warm freshwater environments and some soil around the world. Fowleri is the only species of Naegleria that infects people. Drinking contaminated water cannot infect people and there is currently no evidence that it can be transmitted through water vapor or aerosol droplets.
According to the CDC, the ameba can possibly be found in:
Warm fresh water, such as lakes and rivers
Geothermal, or naturally hot, water such as hot springs
Warm water discharge from industrial or power plants
Untreated geothermal (naturally hot) drinking water sources
Swimming pools, splash pads, surf parks, or other recreational venues that are poorly maintained or don’t have enough chlorine in them
Tap water
Water heaters
Soil, including sediment at the bottom of lakes, ponds, and rivers.
This article originally appeared on Pensacola News Journal: Florida diseases causing alarm include malaria, leprosy and amoeba

