COVID vaccine rollout snarled by insurance denials, canceled appointments
Some consumers trying to get updated versions of the COVID-19 vaccine this week have encountered red tape, canceled appointments and delays getting private insurance to cover the shots.
The major snarl comes amid a systemic shift, as the federal government no longer pays for or distributes all COVID-19 vaccinations. Public and private-sector health insurance providers must pay the full cost of the shot plus an administrative fee. Uninsured patients can still get free shots through a federal government program. In response to an uptick in cases, the Biden administration announced plans Monday to restart another federal program that allows consumers to order four free tests per household.
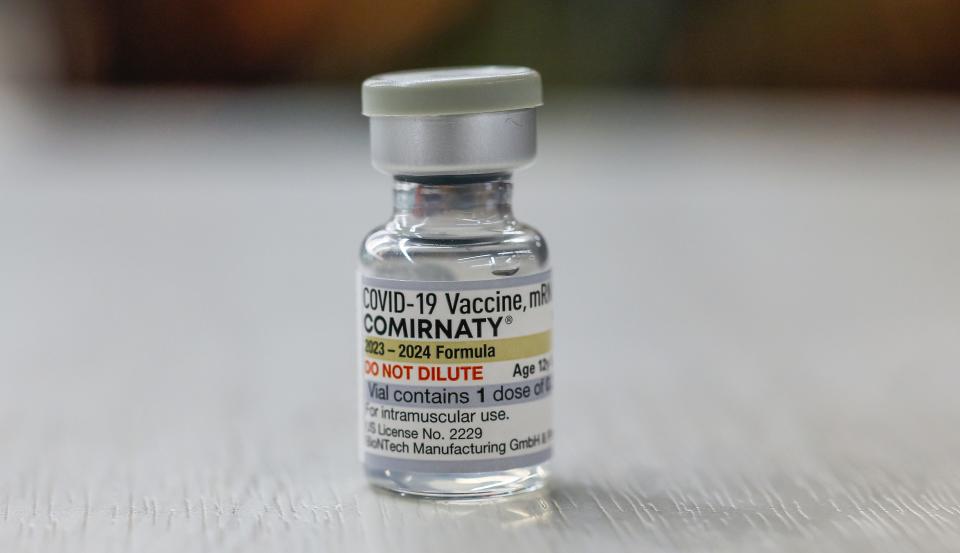
Millions of doses of the updated vaccines from Pfizer-BioNTech and Moderna have been shipped to pharmacies and clinics since the Centers for Disease Control and Prevention approved new versions. The agency has recommended that everyone older than 6 months get updated shots, which target more recent variants of the virus that causes COVID-19.
While chain pharmacies busily give customers their shots, it's been stressful for many people looking to get vaccinated. Dozens have turned to social media to share stories about insurer roadblocks, delays in appointments or out-of-network denials.

Experts say the marketplace is bound to experience hiccups with such a large vaccine rollout shifting from government to private-sector insurers.
"It's pretty much par for the course with the U.S. health care system and the patchwork nature of it," said Sabrina Corlette, founder, and co-director of the Center on Health Insurance Reforms at Georgetown University's McCourt School of Public Policy.
'Very difficult to be responsible'
Patrick Dye, a resident of Vienna, Virginia, began making calls as soon as the new vaccine shots became available but he hit roadblock after roadblock.
When he learned his doctor's office didn't carry the vaccine, he contacted his insurer, Anthem Blue Cross Blue Shield, to ask about options. The insurer told him he'd only be covered if he got a shot from his "health provider" or the doctor, who had already told him his office didn't have the updated shot.

In all, Dye made more than a half dozen calls to his doctor, insurer, a hospital clinic affiliated with his doctor, Walgreens and an independent pharmacy. He finally was able to get a shot Friday at a CVS pharmacy. He said his situation was complicated by the fact that he has a low-deductible, pre-Affordable Care Act health insurance plan, known as a grandfathered plan, which operates under different rules than ACA plans.
Still, he said consumers shouldn't have to work so hard to get vaccinated to protect themselves and others.
"It's very difficult to be responsible," Dye said.
Health expert struggles to get vaccinated
As vice president and director of the ACA at the health policy foundation KFF, Cynthia Cox is well versed in the nuances of the health insurance industry and U.S. health care system.
Yet even she struggled to get a timely shot.
She tried to get vaccinated on Tuesday ahead of a work trip next week, but her health insurer's in-network pharmacies didn't have any vaccines in stock.
She was willing to pay the $200 out of pocket at a Washington D.C.-area Walgreens pharmacy that wasn't part of her insurer's network. When she attempted to do so, the Walgreens employee contacted her insurer, and a representative for the insurance provider informed Cox that she would need prior authorization to get vaccinated out of network. The insurer even requested that Cox track down her doctor's fax number as part of the process.
The end result – Cox didn't get the shot, even though she was willing to pay out of pocket. She couldn't land an appointment at local CVS stores, and staff at a non-chain pharmacy told her they wouldn't get doses until next week.

She searched her insurer's directory of in-network pharmacies that carry the shot, and she found one in Baltimore, a trip "that's not really a solution for the vast majority of people who live in or around Washington D.C.," she said.
"It was ultimately the insurance bureaucracy that kept me from being able to get the shot, despite the fact that I've been working on insurance policy for over a decade," Cox said.
Biden administration, insurers vow improvements
Biden administration officials, health insurers and pharmacies have acknowledged early bumps in the rollout.
A U.S. Health and Human Services Department spokesperson said the agency is aware some vaccine seekers had "unexpected insurance coverage denials at the point of service." The federal agency has reached out to insurers to make sure computer systems are up to date and remind them they must cover COVID-19 vaccines without cost sharing to insured consumers. For the uninsured, the CDC's "bridge access" program will pay for vaccines.
In July, Chiquita Brooks-LaSure , administrator for the Centers for Medicare & Medicaid Services, sent a letter to insurers, urging them to update systems by mid- to late-September to be ready for the vaccine's release.

Health insurers will cover the full cost of the shot "when obtained through a network provider," said James Swann, a spokesman for America's Health Insurance Plans, a trade group that represents major private health insurers. He added that insurers are working with pharmacies and others to "quickly ensure patient access to COVID-19 vaccines with zero cost sharing and address any issues relating to newly added billing codes quickly."
CVS spokesman Matt Blanchette said some insurers' systems aren't yet set up to cover the updated vaccine. In such cases, consumers can pay cash or pharmacy techs can reschedule appointments.
CVS stores have been administering the updated COVID shots since last week and continue to get shipments of doses. Consumers can check CVS.com to confirm whether a store has vaccine doses and make an appointment, Blanchette said.
A Walgreens spokesman said the pharmacy is "committed to ensuring no patient pays and everyone who is eligible and wants a vaccine receives one."
Consumers scramble for shots
Joe Anderson Jr., 36, a health clinic director in Austin, planned to attend the coveted Beyoncé tour in New Orleans next week. To be safe, he wanted to get a COVID-19 booster, even if it wouldn’t provide full protection until a week later.
He found that city, county and federal government websites had little information about boosters, and his private insurance portal and major retailers such as CVS and Walgreens didn't have much either. On Wednesday night, a Walgreens representative called him to say his appointment the next day was canceled, forcing him to scramble for another vaccine in the Austin area.
On Thursday afternoon, he found an appointment at a Walgreens and was unsure whether his insurance would cover it. But when he showed up for the shot, the pharmacy didn't ask him to pay anything out-of-pocket. He then scheduled an appointment Friday for his mother in Dallas.
Though it took a little work and a little luck to find an appointment, his persistence paid off.
“It’s kinda like we have to ask them,” he said. “And it’s really reactionary instead of being proactive.”
COVID cases, testing on the upswing
The new vaccines arrived as COVID-19 infections continued to rise, since early July, but the infection rate remains far below previous peaks. Hospitalizations were up 7.7% during the week ending Sept. 7 and COVID deaths were up 12.5% in the week ending Sept. 16, but totals remain lower than during previous upticks.
In another indicator of concern for public health officials: the share of positive COVID tests climbed from about 4% in early June to over 14% as of Sept. 9. The CDC testing data typically doesn't include home COVID tests unless someone visits a doctor who orders a test through a lab.
Consumers can request their four free COVID home tests per household beginning Monday through the government-run website CovidTests.gov. The federal government plans to award $600 million to a dozen domestic COVID-19 test manufacturers to shore up the government's supply of these tests. The availability comes as chain retailers have reported periodic shortages of home tests.
This article originally appeared on USA TODAY: Consumers seeking COVID vaccine face insurance denials, cancellations

