Decline in US Covid vaccinations presents new problem: how to shrink operations
- Oops!Something went wrong.Please try again later.
A decline in daily Covid-19 vaccination rates has left US public health authorities with a new problem – how to effectively shrink operations.
In the campaign to immunize all American adults against the coronavirus, most of the difficulties to date have involved overwhelming demand and restricted supply. Now, with less than one-third of Americans fully vaccinated, local public health authorities described a sense of whiplash as they pivot from mass vaccination clinics to outreach campaigns, all within a couple of weeks.
Related: US split on vaccine passports as country aims for return to normalcy
“We knew that when folks became eligible the vaccine-ready folks, or eager, [would] come out right away,” said Mary Jo Brogna, director of nursing at Harbor Health Services, which runs a community clinic in Cape Cod, Massachusetts.
“Reaching the final percentage of herd immunity,” believed to be at least 70% of all adults, “is going to be dependent on outreach and addressing any vaccine hesitancy,” said Brogna.
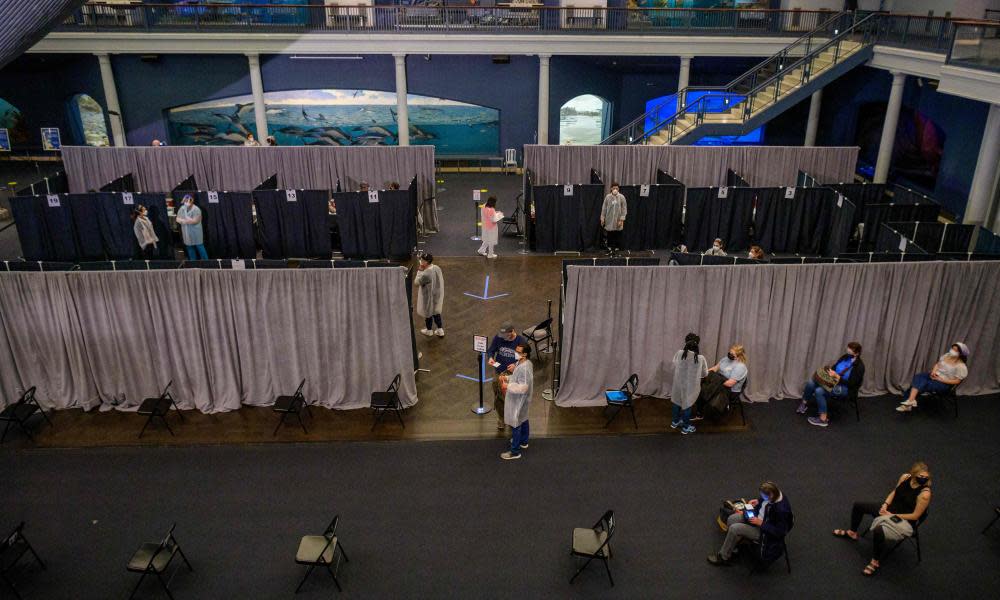
For most of 2021, the story of the vaccine campaign has been overwhelming demand. Emergency authorities took over stadiums, big-box stores and community centers staffed with dozens of nurses and volunteers to inoculate thousands of people per day.
But in the last two weeks daily vaccination rates in the US have peaked and declined from a high of 3.2m daily vaccine administrations per day to 2.5m. Now, health authorities nationally are experiencing what red states such as Mississippi and Wyoming began to see early signs of – a major slowdown.
“Across the country we started out with mass clinics and those mass clinics worked very well for the older individuals,” said Gary Edwards, executive director of the Salt Lake County health department in Utah.
The mass-clinic model is not reaching the segment of the population we’re trying to reach
Gary Edwards
However, he said, “we’ve reached a point, and it’s been very interesting how quick that happened, that the mass-clinic model is not reaching the segment of the population we’re trying to reach,” said Edwards.
The phenomenon is repeated across the country. Local authorities in Los Angeles, California; Colorado; Florida; Nevada and Texas are poised to close mass vaccination sites by the end of May.
Georgia has already decided to shut down all of its mass vaccination sites by the end of May, citing lack of demand. The state is far behind the nation in terms of administering vaccines, with 34% of the population having received at least one dose, compared with 43% nationally.
In Galveston, the public health director apparently inquired about a “pause” in vaccine shipments, as he worried the district would not be able to use all those shipped before they expire.
The reasons for the slowdown are nuanced, most experts said.
Vaccine hesitancy, especially among conservatives and racial minorities, is playing a role. But so too are difficulties with scheduling and transportation, as working-aged adults have fallen far behind older adults in terms of vaccination rates.
One of the most notable trends in the immunization campaign is the relatively low rates of vaccination among adults aged 18-49. In this age group, 9-12% of people are fully vaccinated, compared with more than 27% among people aged 50-64.
“I had a patient the other day where I was trying to go through the process of online scheduling with him and we just kept hitting a wall,” said Dr Ann Chahroudy, a pediatric infectious disease specialist and faculty at Emory University in Atlanta, Georgia.
Crucially, his also might be one of the most important groups to vaccinate. In summer 2020, research in the journal Science found that working-aged adults 20-49 were the most likely to transmit the disease to more than one person.
“Thus, working adults who need to support themselves and their families have fueled the resurging epidemics in the United States,” an international group of researchers concluded. The same age group appears to be driving cases now in states such as California and Utah.
Also notable is the lack of uptake in conservative regions. Data from the CDC shows states across the south and west have the highest levels of vaccine hesitancy, and uptake is notably low across these states. Multiple polls have now found Republicans are more likely to say they will not get vaccinated.
“Reaching those young Republicans and conservative groups becomes a priority, because it’s the difference between normalcy or something less,” said Dr Peter Hotez, a vaccine researcher and the dean of the National School of Tropical Medicine at Baylor College in Houston, Texas. Lack of vaccine uptake, he said, “is not going to be homogeneously distributed. That means Covid-19 becomes a red state disease”.
The politicization of the pandemic and dismissal of science on the right, especially by Donald Trump, has led many influential conservative pundits to question Covid-19 public health measures – from Fox News’s Tucker Carlson to the influential podcaster Joe Rogan.
“We’ve got to rip the anti-science out of the Republican party,” said Hotez. “We have to help our conservative brothers and sisters.”
High levels of vaccine hesitancy are also being blamed for imbalances in supply and demand, such as in Illinois. But, as Cape Cod shows, the whole story is much more nuanced.
Barnstable county, known regionally as the Cape, has the lowest rate of vaccine hesitancy in the nation. Just 6% of residents there are believed to be somewhat hesitant, according to data from the US Centers for Disease Control and Prevention (CDC).
The county has administered more shots than any other in Massachusetts, and 59% of people here have received at least one vaccine dose, compared with 43% nationally. In no uncertain terms, it’s a success story. Nevertheless, demand has also stalled at Brogna’s clinics, and public health authorities there are still trying to figure out why.
“We’re surveying our own patients,” said Brogna. “We’re reaching out and looking at patients who have not been vaccinated to say, ‘Gee we’ve contacted you three times and noticed you haven’t scheduled a Covid vaccine. Can we talk about it?’” she said.

