Michigan doctor begs for more help as state tops COVID-19 hospitalization peak
- Oops!Something went wrong.Please try again later.
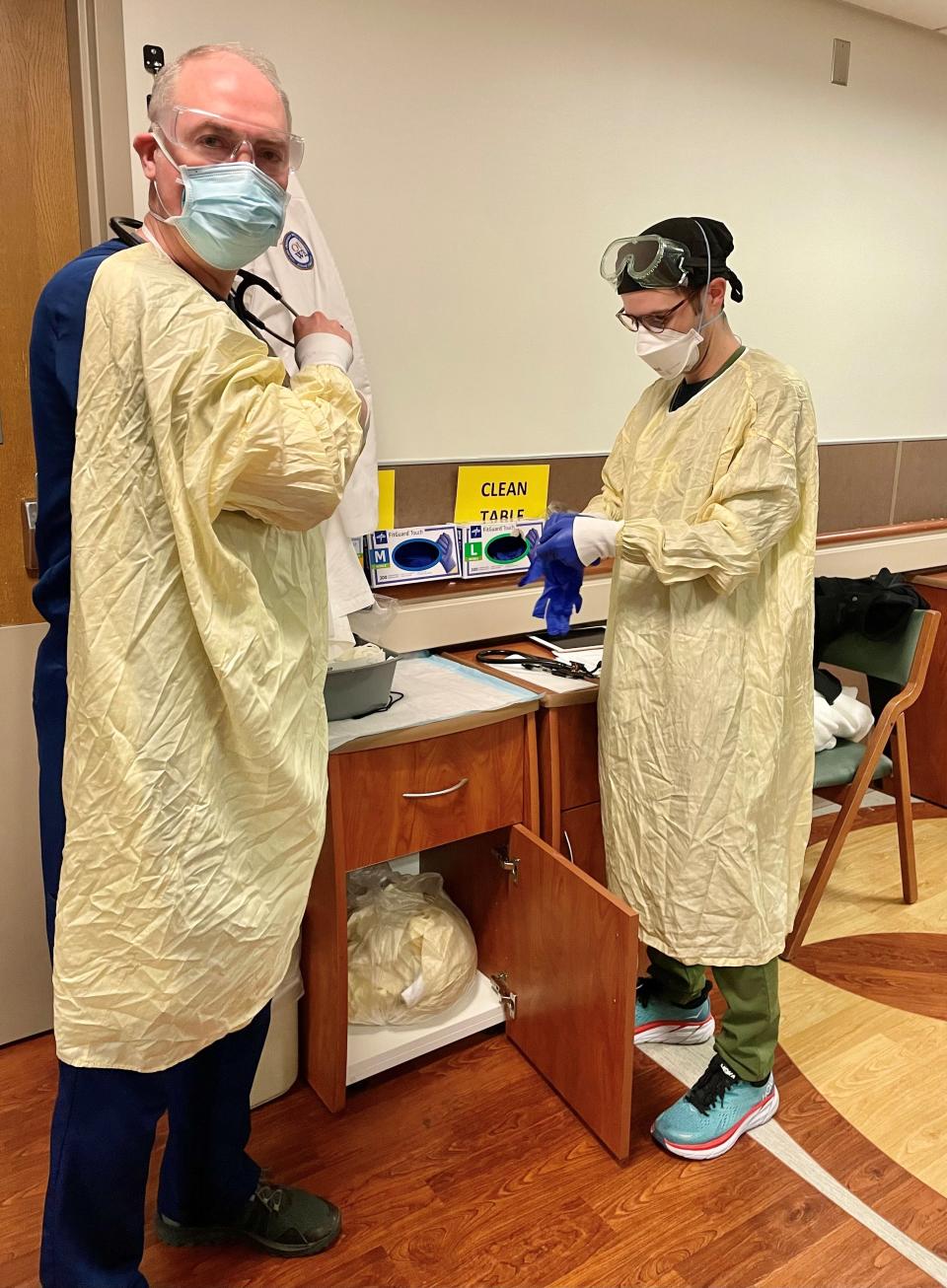
As Michigan broke another pandemic record Monday — this time for confirmed COVID-19 hospitalizations — a critical care doctor called on the state and federal governments to "bring to bear all resources" to help the hospitals ride out the worst-yet surge and for health care workers who've left medicine to return to the field.
"Health care is stretched incredibly thin," said Dr. Paul Bozyk, section head for pulmonary and critical care medicine at Beaumont Hospital in Royal Oak and vice chair of the board of the Michigan State Medical Society.
"The numbers are significantly picking up in the community and health care is bearing the brunt of that."
Even though the federal government already is sending three emergency medical strike teams to hospitals in Saginaw, Grand Rapids and Dearborn to help in pandemic relief, it's not enough, Bozyk said.

"We need the next (team) and the next after that," he told the Free Press in a series of wide-ranging interviews over the last week about the critical short staffing and stress COVID-19 and other illnesses are putting on health care workers.
"And we need people that may have taken a hiatus from health care for their own personal, physical and emotional health to consider a return so that they can rejoin us on the front line to try to get us through this very challenging time."
As of Monday, 4,404 people were admitted to Michigan hospitals with confirmed cases of the virus. Of them, 40 were children, according to Michigan Medicine, which supplies the state health department with hospitalization data.
That breaks a pandemic record set on April 8, 2020, when 4,365 people were hospitalized with the virus during an initial surge that had the nation reeling as so little was known about the virus, how it spread and how to treat it.
More: Michigan's new top doc on pandemic response: 'None of this should be political'
More: Michigan hospitals near breaking point with COVID-19, other patients
"There's COVID and we're already in this surge that's concerning. On top of that, we're seeing flu outbreaks," said Dr. Natasha Badgasarian, chief medical executive of the Michigan Department of Health and Human Services. "We're seeing circulating influenza and we know that flu season is upon us, imminently upon us and the hospitals can't take any additional strain.
"We're asking for assistance from the federal government. We're asking for assistance from partners working together ... with the health systems. But we're really entering a critical phase."
Bagdasarian, who also is an infectious disease epidemiologist, said she meets with the chief medical officers of the state's health systems weekly "to talk about how we're going to handle some of this load and some of this strain, how do we share the burden, how do we work together cooperatively to make sure that Michiganders are getting the best medical care that they can."

More: Michigan shatters peak COVID-19 case rate. 1 in 10 cases in US are from the state
More: Feds to send staff to Michigan hospitals to treat COVID-19 patients as pandemic rages
In addition to deploying the three federal emergency teams of health care workers to Covenant HealthCare in Saginaw, Spectrum Health Butterworth Hospital in Grand Rapids and Beaumont Hospital in Dearborn, five other hospitals also have been applied for federal aid and received validation for similar assistance.
They are:
Mercy Health in Muskegon
Munson Healthcare in Traverse City
Bronson Methodist Hospital in Kalamazoo
Sparrow Hospital in Lansing
Beaumont Hospital in Troy
However, it's unclear how long it might take for help to come to those hospitals, if it does at all. That's because every state is competing for the same share of federal resources.
Additionally, the John D. Dingell Department of Veterans Affairs Medical Center in Detroit is opening beds to take transfers of civilian patients for at least the next 30 days. And the Michigan National Guard has been deployed and is "playing a role in a variety of areas," Bagdasarian said.
Without more help, Bozyk said he's not sure that all Michiganders will get the care they need.
"The glass can only hold so much water and at some point it's going to overfill and it's overfilling in several hospitals across the state ... right now," he said.
"Hospitals across Michigan are going to have to make really difficult choices on how to best use those increasingly scarce resources ... with the increasing severity of illness. That certainly can include things like delaying elective procedures that require an inpatient stay."
But it could become a slippery slope.
"It begs the question of what's next after elective procedures?" he said. "Do we delay urgent but not emergency procedures and then what if there's no beds for the urgent procedures? I know of colleagues in other hospital systems that are delaying important heart surgeries because they have no bed to take the patient to post-operatively.
"So it's a waiting game. Will a bed open up before something terrible happens to this poor patient? And these are the very difficult times that we deal with."
Bozyk is especially concerned about rural Michigan, where small community hospitals already were operating with tight staffing and limited ability to handle critically ill patients. Now, they're having a difficult time finding larger, higher-acuity hospitals that are able to accept those patients as transfers.

More: Michigan coronavirus cases: Tracking the pandemic
"I just don't know how they are going to cope with this fourth surge unless something is done and done immediately," Bozyk said. "I believe that ought to include any state or federal resources that can be brought to Michigan to help our health care system weather this crisis that's increasing by the day.
"It's terrible. It's terrible because we are founded on the principle that we want to help everyone. But clearly when resources are strained, we cannot and that's tragic."
He worries an already high death toll from COVID-19 could grow higher — even among people who might have been saved had there been more health care workers and more available hospital beds.
"The risk for death and dying increases the more a hospital is strained," Bozyk said. "So when we see surges within the pandemic, it's frustrating because we say why can't we get our community vaccinated? Why can't we help educate people to make the right choice? Because it's incumbent upon each person to make the right choice for their family and their community so they don't have to come to the hospital and then are not a strain on resources."
Bozyk gets emotional talking about patients who refuse COVID-19 vaccines and end up on ventilators. The decision to opt out of vaccines affects more than just that individual.
"Please don't only think of yourself because in the hospital right now, I see way too many pregnant women with COVID infection," he said. "I see way too many parents with young children in the ICU (intensive care unit). And these are children that may not grow up to know their parent because of the choice their parents made."
More: Public health advisory for Michigan amid COVID-19 surge: Wear a mask
More: COVID-19 hospitalizations climb in Michigan as nation braces for emerging omicron variant
When a person gets so sick they need to go on a ventilator, he said most ask for a vaccine. But, he said he tells them: "First, we'll get you through this. Then, we'll get to your vaccine.
"There's a tremendous amount of fear, and I can share just the most terrible stories about dialing the phone ... for people so they can talk to their loved ones before they go on the ventilator, and it's so sad. It's so sad."
But he keeps going back to work each day.
"You do it for the victories because if there wasn't a team of dedicated health care workers to help these patients in their greatest time of need, the fatality rate would be exponentially higher."
Unvaccinated patients are less likely to survive and come off the ventilator, he said, especially if they have underlying health conditions.
"Too many times I've heard, 'I'm not going to get vaccinated. I have COPD, so I'm not going to get vaccinated.' These are exactly the people that need to get vaccinated, that must get vaccinated to ensure they can stay safe (in) this pandemic to the maximum extent possible."
About 55% of the total Michigan population has been fully vaccinated for COVID-19. That compares with 60% nationally, according to the U.S. Centers for Disease Control and Prevention.
It's disheartening, Bagdasarian said.
"We all know what works," she said. "We all know that the pillar in 2021 in terms of stopping COVID transmission are our vaccines. These are incredibly safe and effective vaccines. And one of the sad things is we have not seen uptake of vaccines the way (we'd) like."
The rate of flu vaccinations in Michigan also is well below the goal, she said.
"We are not anywhere close to our target for influenza vaccine doses," Bagdasarian said. "We would like to get to 4 million doses and we're just over 2 million. We need to get our citizens vaccinated for not just COVID, not just get their COVID boosters, but get their flu boosters.
"Reducing community spread of COVID ... reducing community spread of influenza, that's really what we need to focus on now in order to help our health systems take care of us."
Bozyk said people also need to take other steps now to slow the spread of the virus — such as wearing masks and avoiding gatherings and crowded indoor places with poor ventilation.
"Until we see that infection rate start to downturn, we're going to see a climbing number of cases," he said. "When we see a climbing number of cases we're going to see an increased number of hospitalizations. When we see increased hospitalizations, we're going to see increased admissions to the ICU. And, unfortunately, given the mortality rate of this virus, that translates into an increased number of deaths for a potentially preventable condition.
"Things are likely to get worse before they get better."
Cary Junior, Free Press audio producer and the host of the "On the Line" podcast, contributed to this story as did reporter Kristi Tanner.
Contact Kristen Shamus: kshamus@freepress.com. Follow her on Twitter @kristenshamus.
Subscribe to the Free Press.
This article originally appeared on Detroit Free Press: Doctor begs for help as Michigan tops COVID-19 hospitalization peak

