Dr. Dwelvin Simmons: Innovative treatments can help turn the tide against prostate cancer
The American Cancer Society’s 2023 cancer statistics report was released in January. It detailed some very encouraging trends. For one thing, the report found that overall cancer mortality has declined by 33% since 1991. That’s more than 3.8 million cancer deaths averted.
Another highlight: Cervical cancer incidence among women ages 20-24 plummeted by 65% between 2012 and 2019. We should credit this result to the successful introduction of the HPV vaccine for girls and young women.
At the same time, the report found a troubling reversal in a long positive trend around prostate cancer, the second-most common cause of cancer death among men. After decades of decline, prostate cancer incidence increased 3% a year between 2014 and 2019. This was driven by an increase in diagnosis of advanced-stage prostate cancer, which increased between 4% and 5% annually since 2011.
Donna Deegan:Honoring countless miles run, looking forward to breast cancer-free future
Jacksonville patient gives back:Local cancer survivor funds oncology support program to help with non-medical needs
This trend included the years of the COVID-19 pandemic when many patients put off routine screenings. Now that we are emerging from the pandemic, we are treating patients with advanced cancers that could have been detected and diagnosed earlier under normal circumstances.
Prostate cancer is a disease that affects the prostate, which is a small walnut-shaped gland located just below the bladder in men. The prostate gland produces the fluid that nourishes and transports sperm.
In Florida, the National Cancer Institute reports a current prostate cancer incidence rate of 97.9 per 100,000 with a mortality rate of 16%. Florida ranks second in predicted prostate cancer incidence and mortality, with more than 162,000 new cases and more than 47,000 deaths estimated to occur in 2023, according to the American Cancer Society’s Cancer Statistics Center.
About 1 in 8 men will be diagnosed with prostate cancer in their lifetime — and about 6 cases in 10 are diagnosed in men who are 65 or older. Given that Florida has the second-highest number and percentage of residents 65 and older, the prostate cancer burden in the state is relatively high. Prostate cancer disproportionately affects African American men, who are more than twice as likely to develop prostate cancer and to die from the disease.

Advanced prostate cancer, also called metastatic prostate cancer, means the disease has spread to other parts of the body. Whereas prostate cancer is highly treatable if it is detected early, advanced prostate cancer is more challenging to treat.
Fortunately, innovative diagnostic and therapeutic methods are improving how we can detect and treat advanced prostate cancer. These novel modalities are becoming more widely available, even in communities that don’t have an academic medical center or large urban hospital. The key is raising awareness and offering support to connect at-risk patients to appropriate care close to home.
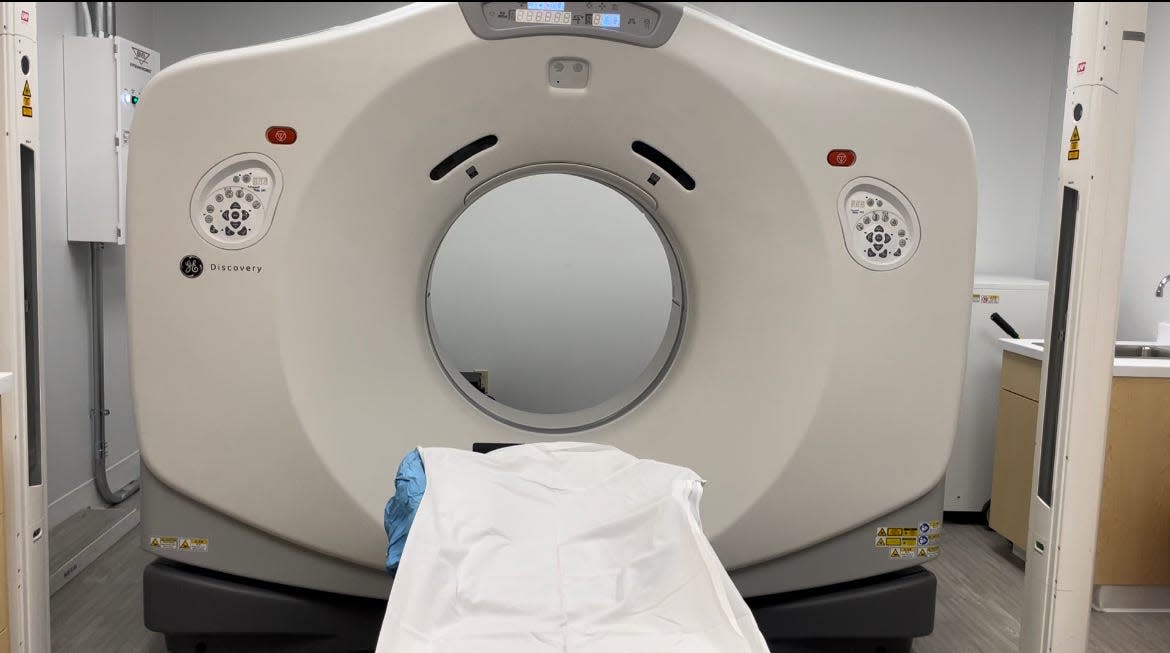
PSMA PET is at the forefront of these efforts. This diagnostic modality is most effective for localizing metastatic prostate cancer in men who have already been diagnosed, in order to further assess the severity of the disease. With PSMA PET scans, targeted imaging is used to detect areas of suspected metastasis for initial therapy and recurrence based on an elevated serum prostate-specific antigen (PSA) level. (If “PSA” sounds familiar, that is because the PSA test is commonly used in regular screenings for prostate cancer.)
The PSMA scan utilizes two common types of scanning technology — positron emission tomography (PET) and computed tomography (CT) — as well as a special radiotracer. The radiotracer is injected into the body prior to the scan and is attracted to a substance in the body called prostate-specific membrane antigen (PSMA). PSMA is a protein found on the surface of prostate cancer cells, including those that have spread outside of the prostate itself. The tracer then can be detected by the scan, showing where the cancer has spread.
'Second chance at life':Jacksonville nonprofit educates minorities about organ donation, transplants
These results provide extremely detailed information to help physicians detect prostate cancer more easily, as well as to plan effective, personalized care strategies.
PSMA PET is part of a novel approach called theranostics, a term that combines “therapeutics” and “diagnostics.” When warranted, patients can be treated with precision radiopharmaceutical agents. A radiopharmaceutical called Pluvicto, for example, is now being used to treat a type of advanced prostate cancer called prostate-specific membrane antigen–positive metastatic castration-resistant prostate cancer (PSMA-positive mCRPC for qualifying patients).
The impact has been significant: Across the GenesisCare network in the U.S., more than 1,700 patients have benefited from PSMA PET and theranostics since 2021.
Turning the tide against advanced prostate cancer begins with raising awareness among at-risk populations and connecting them with opportunities for early detection. Improving outreach and support for these men will improve their access to a personalized care approach and should help reverse the negative trends detailed in the American Cancer Society’s 2023 report.
Dr. Dwelvin Simmons is a radiation oncologist who practices with GenesisCare in Jacksonville.
This guest column is the opinion of the author and does not necessarily represent the views of the Times-Union. We welcome a diversity of opinions.
This article originally appeared on Florida Times-Union: New tech offers hope for those at risk from prostate cancer

