Emergency medicine: Burnout from COVID-19 pandemic has resulted in rise of travel nurses
As I walked through the emergency department a few days ago I realized I didn't recognize many of the staff who were working. I have been an emergency physician in my current job for more than 10 years and usually know most of the team. Over the years, I have seen staff members advance their careers, get married, have kids and move out of state or to another country, but I have never seen it like this. I sat next to a nurse I have known for a long time and asked what was going on. The nurse, Beth, sighed and asked if I really wanted to know.
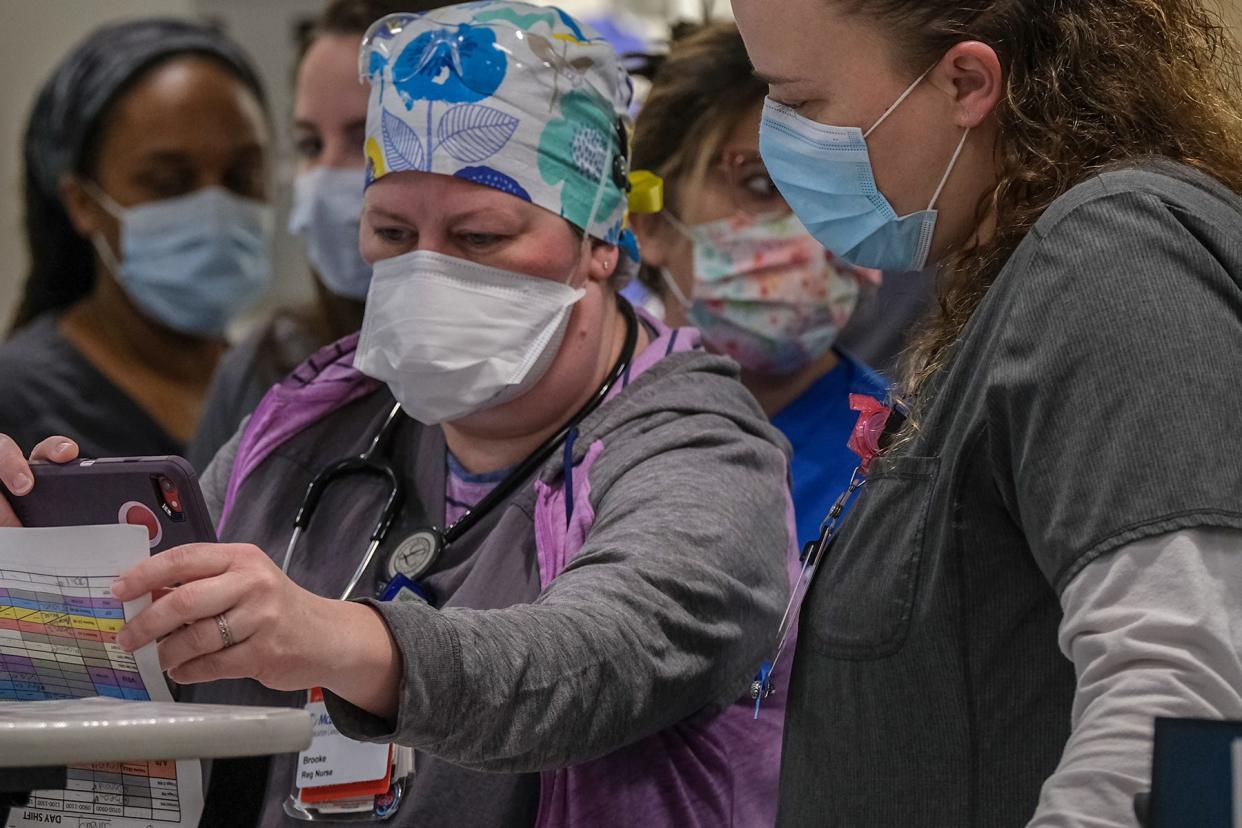
She told me that more of our staff nurses had recently left and there was a new group of travel nurses who had just started. There have always been travel nurses, who work in short-term roles. However, the need for travel nurses has grown significantly in recent years due to a combination of factors. As our staff nurses have left for various reasons, our hospital and emergency department (like many others across the country) have had to fill the gaps with travel nurses.
Even before the COVID-19 pandemic, there was a nursing shortage. But the repeated surges of the coronavirus over the past few years have significantly worsened things. Many nurses have retired early or left the field due to burnout and moral distress. The nurses that are left are working with understaffed units and continually increasing volumes of patients.
These nurses are increasingly stressed and burned out and many are looking for a way out. Hospitals have relied on travel nurses to fill vacancies, but the nursing shortages continue and the health-care system is facing unprecedented stress during one of the worst public health crises in our history.
Travel nurses get paid higher wages than staff nurses because they lack all the perks that come with a full-time job such as job security and benefits and they have the inconvenience of traveling and working in different locations for short periods. Beth said she doesn't mind travel nurses making more money than she does and is just grateful to have the help.
Despite our efforts to add staffing in creative ways, the lack of nurses is visible to me every day. When there aren't enough nurses to staff hospital or emergency department (ED) beds, those rooms go unfilled. This leads to a backup of patients. If there are no available beds in the hospital, patients will have to wait for their ED beds. Once the beds are filled, other patients who come into the ED have to wait in the lobby. Our triage nurses evaluate each patient who comes in and determine how sick they are. The sickest, or most potentially sick, are seen more quickly than those with less acute complaints, which these days can mean a lengthy wait.
After talking with Beth, I saw my next patient who had just been transferred from a rural community hospital for stroke symptoms. Bill had presented to the other hospital emergency room two days earlier and had been evaluated by our virtual stroke team. He had developed left-sided weakness and slurred speech 20 hours before he went to the hospital. Bill wasn’t a candidate for any acute intervention including the clot-busting medications that must be given within hours of symptom onset. The rural hospital did not have a neurologist available to see Bill in the hospital, so he was transferred to my hospital so he could be admitted to our ED and undergo additional testing.
Unfortunately, because our hospital was so backed up with no available beds, Bill had to wait in the other ED for two days before he was transferred. He was understandably frustrated by having to wait so long. While nothing detrimental happened to him while he waited, he also was not getting the care he needed. He was very abrasive to the nurse as she checked him in and told me he wasn’t interested in answering any of my questions. His wife came in a short time later and was able to calm him down. He apologized for his behavior and explained that he was just frustrated and felt like he had fallen through the cracks. I could sympathize with Bill; I am equally frustrated by these situations.
These types of scenarios unfortunately are common these days. It seems like most days and nights are busy and it is affecting the whole health-care system. I see patients and families having to wait while they're uncomfortable and scared. I see the frustration and fatigue wearing on my colleagues. I wonder how long this can continue.
I still see amazing teamwork and patient care despite many challenges beyond our control. We all need to be patient and understanding of each other and continue to do our best every day. My colleagues continue to show up and I am proud to work alongside them as we hope things get better.
This article originally appeared on The Columbus Dispatch: Hospitals struggle with not enough nurses, backup of patients

