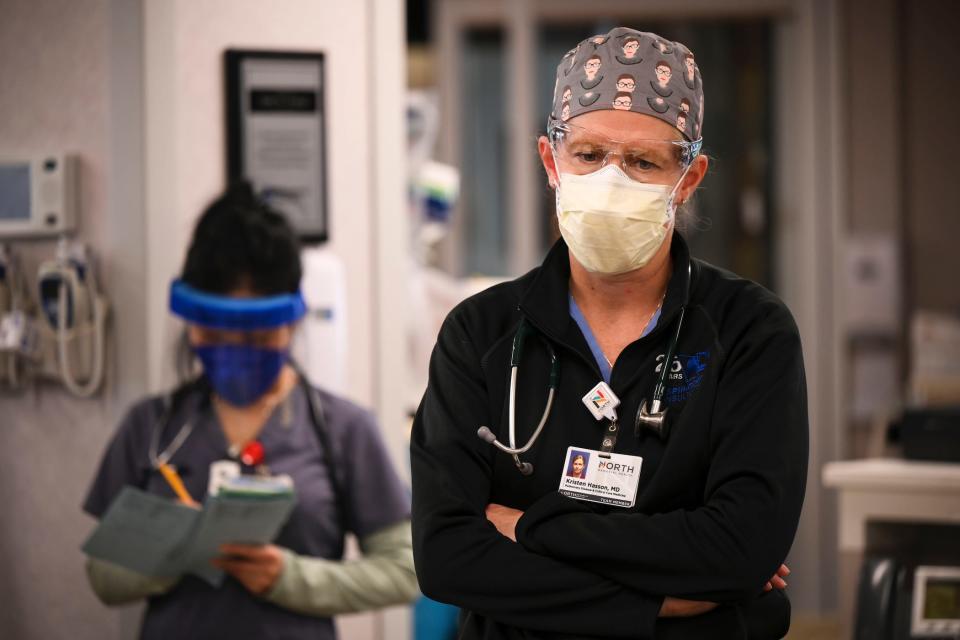
ER doctors say this COVID-19 wave is forcing them to deny treatment to other patients who can die as a result: 'Every shift I'm working these days is like the worst shift in my career'
Top ER doctors in several states say they're being forced to refuse life-saving care to patients.
About 30 to 40% of their beds are tied up with COVID-19 cases.
"We say no day after day," one ER doctor said. "And that's led to preventable deaths."
There is not enough room for all the sick and injured people in Minnesota to receive the emergency care they need.
Hundreds are waiting, some on the floor, in hopes that a bed or operating table might open up. On Tuesday morning, 246 patients statewide had been waiting for more than four hours for a bed.
It's a backlog created by yet another surge of COVID-19 cases. Doctors and nurses say there's no end in sight, and people are likely dying in the shadows of this wave of infections.
Dr. John Hick, the medical director for emergency preparedness at Hennepin County Medical Center, told Insider his colleagues are examining people's ankles who are sitting on the floor, because they have "literally run out of any space to put them."
Medical teams from the Department of Defense have been brought into his hospital to help deal with the overflow. These days, all 50 beds in the department are filled, with up to 70 more patients waiting for care in the triage area at any given time.
"Every shift I'm working these days is like the worst shift in my career," the 25-year emergency-room veteran told a group of journalists last week.
"We're electing to have to leave patients in rural hospitals" and discharging patients "that I normally would've admitted," Hick told Insider, calling it a "first-come, first-served" system, which is not how emergency medicine is supposed to work.
It doesn't have to be like this anymore, Hick said. Last week, his hospital system, along with eight others across the state, took out a full-page newspaper ad urging people in Minnesota to get vaccinated. Almost all of his hospitalized COVID-19 patients are unvaccinated, he said. Like other providers across the country, he has seen the effect vaccines can have on disease severity, and he knows that severe sickness and hospitalization from COVID-19 is by and large preventable today.
"We're very worried about the potential that we're going to have lives that'll be lost," Hick said.
This COVID-19 wave 'has led to preventable deaths,' doctors say — and it's not all from the disease
It's a problem playing out in spots around the country as COVID-19 patients spend weeks, if not months, in their hospital beds.
While the average hospital patient might use a bed for two to five days, hospitalized COVID-19 patients require at least a week or two of care, Dr. Nathalie Dougé, a traveling hospitalist who has worked in both New York City and Montana, said. Often, COVID-19 stays can stretch far beyond that, topping well over a month in the intensive-care unit as a patient's lungs and body recover from the viral illness.
"Getting those extra beds to help other people isn't happening," Dougé said.
Across Rhode Island, upstate New York, and in Iowa (where elective surgeries are on pause through Christmas), hospitals are stretched to the breaking point. In states including Montana, Minnesota, and Nebraska, that routinely means critical care is being denied to rural patients at smaller hospitals.
"When a doctor from a small town in Nebraska calls and says, 'I need some help' ... in many instances, now we've had to say, 'I'm sorry, but we just don't have the capacity to care for that patient,'" Dr. Mark Rupp, the medical director of the University of Nebraska Medical Center's department for infection control, told Insider.
Rupp said, "It runs very much counter to our culture here."
"We've always served as a backup, caring for the sickest of the sick," he said. Today, the hospital is so overfilled that they can't, he added.
Dr. Matthew Prekker, a critical-care and lung specialist who works alongside Hick in Minnesota, put it more bluntly. He said there was no doubt in his mind that people have died because his hospital simply didn't have enough space for them.
"We have historically been the place where people that have nowhere else to go can come," Prekker said, adding that critically injured patients from all over the state requiring specialized care would normally "be on a helicopter to our facility within an hour."
"Now, we say no day after day," Prekker said. "And that's led to preventable deaths."
Hick said he worried about whether any life-saving extracorporeal membrane oxygenation (ECMO) heart and lung machines would be available this winter if someone fell through the ice or got stuck in the snow. When that happens, people can freeze to death within hours. But ECMO machines can help prevent those deaths — if they're not all being used on COVID-19 patients.
"As long as it hasn't been hours and hours, we can often get those people back and discharge them neurologically intact using ECMO," Hick said. "But we don't have the option to do that when we don't have any circuits."
In 2019, at least 62 Minnesotans died cold-related deaths, but the figure would likely be much worse without ECMO machines. There are only four adult ECMO centers in Minnesota, and they're often at or near capacity these days, the Minnesota Department of Health said.
'People still think, "It won't be me"'

In Minnesota, about 43% of state ICU beds were filled with COVID-19 patients as of Monday morning. At this point in the pandemic, many being admitted are relatively young and unvaccinated.
"The great majority of patients I see have been vaccine refusers," Prekker said. On his shift Tuesday, he said he saw "a half dozen young adults that had chosen not to be vaccinated and came in with COVID."
Their admittance quickly creates a backlog in ER departments — as more new patients need care, there are no inpatient beds left to send them to. On top of that, gunshot and stab-wound victims are surging toward record numbers in Minnesota this year.
"There's a level of anger and frustration in the community that I've never seen before," Hick said. "And if people get angry, and they've got a gun, the guns are going off."
At Hennepin County Medical Center, even some of the pediatric beds are filling up with adult patients, Prekker said. It's created a situation where if a rural child needed to be flown in for help, the hospital wouldn't necessarily be able to take them "because sick adults are taking those beds," Prekker added.
It's both heartbreaking and exhausting for the doctors.
"People still think, 'It won't be me,'" Prekker said. "They're willing to play the odds and can think of a whole lot of rationale why they don't need to take the personal responsibility to get fully vaccinated."
Often these days, he said, "one of the last things they say before we have to intubate them and put them on a ventilator is, 'Can I get the vaccine?'"
Meanwhile, other patients wait.
"You have to tell the family that we just have to play the waiting game and hope and pray that somehow some way, we can find a place for them," Dougé said, describing the process of calling up larger hospitals across Washington, Idaho, and Utah, none of them with any room for critical patients from Montana.
"You do feel betrayed to some degree by the community," Rupp said. "We've been working overtime for so long in order to try to preserve their health. And they're not taking the simple step of getting vaccinated."
Be careful 'because the care that we would love to give you, it is severely hindered by exhaustion'
The winter COVID-19 wave has not hit everywhere as hard.
In New York City, the pace of COVID-19 hospitalizations is manageable, Dr. Bruce Farber, the chief of public health and epidemiology at New York's largest hospital system, Northwell Health, told Insider. Elective surgeries continue in the city, and beds are readily available.
But the Omicron variant is taking off fast.
With more than 80% of New Yorkers vaccinated, Farber said he didn't expect the hospital to be overwhelmed with severely sick people. Instead, he said he anticipated a lot of people — including frontline workers — would test positive and have to isolate at home. That, in turn, would mean fewer staffers available to treat patients who are in the hospital.
"I do think it's going to be a real rough six weeks for sure," Farber said.
For Dougé, whose experience working in New York City during the dawn of the pandemic was recently chronicled in the documentary film "The First Wave," the hours and pay as a staff doctor became untenable during this crisis. Now, she said she earned as much in a week as a traveling doctor as she used to make in a month on staff at Northwell.
"I don't see myself going back to a full-time employee," she added. "I know that's going to get exploited."
Her advice to would-be patients is simple: Be very, very careful.
"Honestly, what I tell people: This is the best time to be in the best shape of your life," she said. "Don't do anything risky.
"This is not the time to be in a motor-vehicle accident because the care that we would love to give you, it is severely hindered by exhaustion, by understaffing, limited resources. No matter what we can do as an individual, collectively, the system is on the brink."
This story has been updated with the latest information from the Minnesota Department of Health on ECMO capacity.
Read the original article on Business Insider

