When will the fall booster shot come out? What to know about COVID, RSV in Illinois
As some Illinoisans look forward to cooler temperatures and the beginning of a new school year, residents will also contend with respiratory viruses, which are “more likely to spike in colder seasons,” according to researchers with Harvard Medical School.
Early August has seen a 14% spike in new COVID-related hospital admissions across the nation, according to data from the U.S. Centers for Disease Control and Prevention. Although hospitalizations had a significant increase recently, the number is still far below the coronavirus pandemic’s peak, ABC News reported Aug. 15.
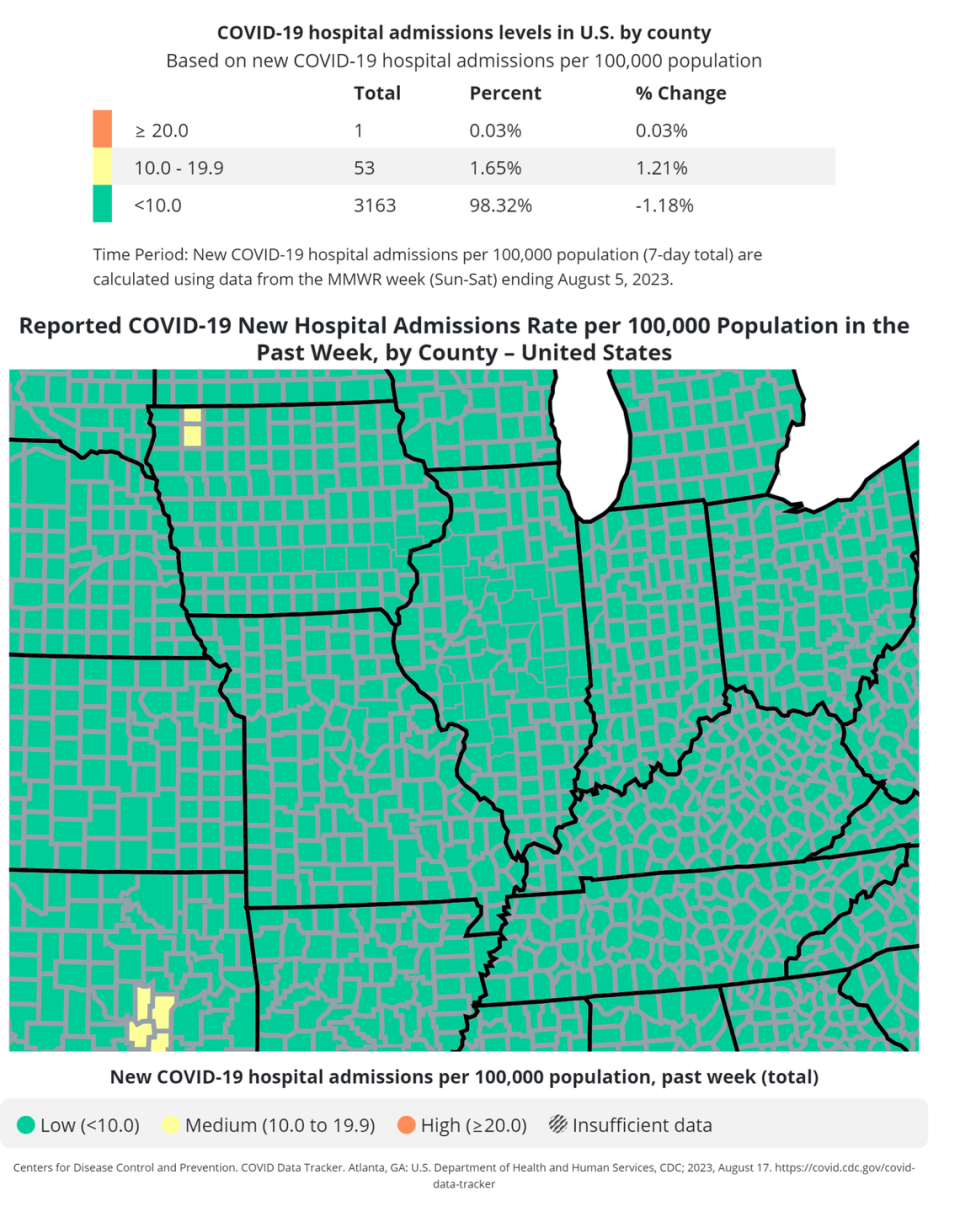
All counties in Illinois are at a low community level for COVID-19, according to the CDC’s map. The reporting metrics changed in May with the end of the federal COVID-19 public health emergency.
While community levels previously considered case rates, hospitalizations and the portion of staffed inpatient hospital beds in use by patients with COVID-19, the CDC no longer tracks COVID-19 cases. Now, a county is at a low level if fewer than 10 residents are hospitalized per 100,000, a medium level if there are between 10 and 19.9 hospitalized and a high level with more than 20 hospitalized per 100,000 residents.
Dr. Vidhya Prakash, chief medical officer and associate dean of clinical affairs and population health at Southern Illinois University School of Medicine, told the News-Democrat the state’s metrics looked good as of early August, but it’s important officials continue monitoring them.
Here’s what to know about COVID-19 and respiratory syncytial virus, commonly known as RSV, this fall in southwest Illinois.
COVID-19 in Illinois
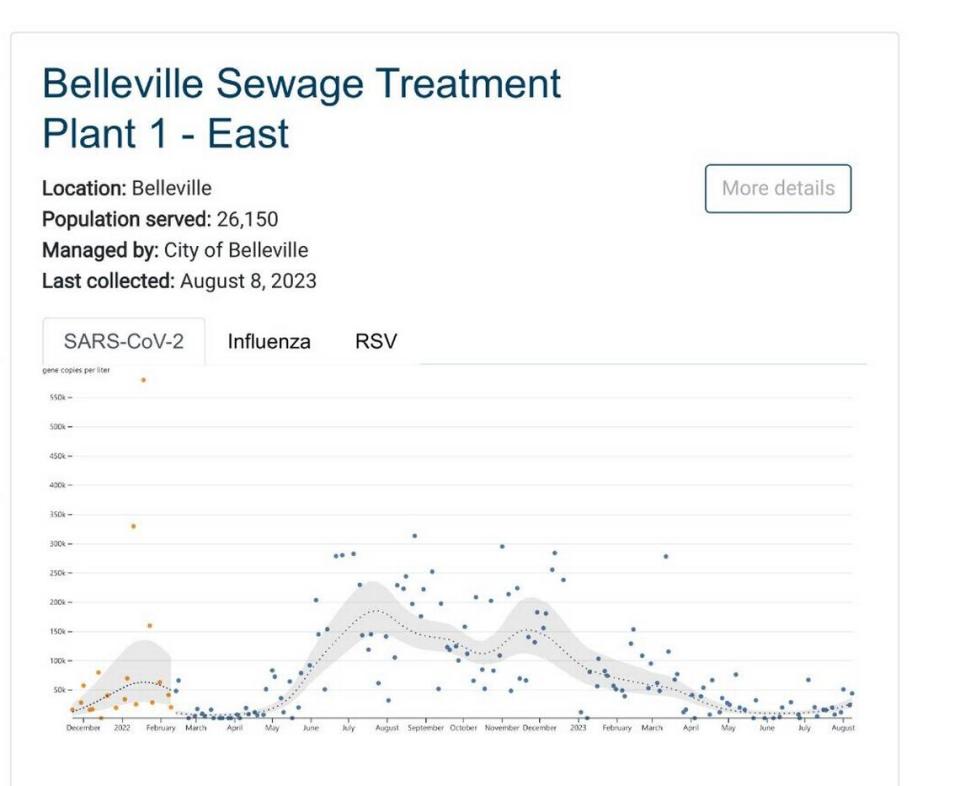
The primary metric now being used to evaluate COVID-19 spread in Illinois is the state’s wastewater surveillance system, Prakash said.
Data is available for sewage treatment plants in Belleville, O’Fallon, Sauget, Edwardsville and other Illinois locations. In addition to COVID-19 data, researchers also track samples of RSV and influenza. The information is presented in scatterplots, with dots representing the number of virus gene copies per liter of sewage.
Recent data from Belleville’s sewage treatment plant shows COVID-19 gene copies are up from June and July, but much lower than in December through March.
As colder months approach, U.S. Food and Drug Administration officials have provided advice to vaccine production companies asking them to make monovalent vaccine boosters available this fall, specifically to protect against the XBB lineage of the omicron variant, Prakash said.
The last COVID-19 booster was bivalent and geared toward protecting against the original COVID-19 strain, as well as the omicron variant.
“I think another booster is definitely on the horizon,” Prakash said.
As of February, the omicron subvariant XBB.1.5 was the dominant COVID-19 strain in much of the U.S., the American Medical Association reported. The subvariant spreads more easily than others, even among those who have been vaccinated and/or previously infected, according to the AMA.
Updated COVID-19 vaccines should be available by late September, CBS News reported Aug. 9.
RSV in Illinois
RSV, another common virus in chillier months, typically causes mild, cold-like symptoms in patients. But many Illinois residents have faced complications from the disease, including pneumonia.
There was a “significant peak” in RSV last October, according to the Illinois Department of Public Health. The disease overwhelmed hospitals across the state, and some health care facilities primarily serving adults temporarily converted beds for older children to reserve pediatric beds for younger children. At one point last fall, only 6% of pediatric intensive care unit beds were available in Illinois, according to an October report from the state health department.
Respiratory Syncytial Virus (#RSV) can cause serious illness in older adults, especially those with certain medical conditions or other risk factors.
If you are 60 or older, talk to your health care provider about whether an RSV shot is right for you: https://t.co/ZxutONBk3G pic.twitter.com/TtmvbfP5ll— CDC (@CDCgov) August 16, 2023
There are two RSV vaccines recommended to people over the age of 60, Prakash said, but patients should confer with their primary care physician to determine whether they’re a good candidate for the vaccine.
The FDA approved one of the RSV vaccines, Arexvy, in early May, while Abrysvo was approved just a few weeks later.
An ongoing study of Arexvy showed the vaccine reduced the risk of developing RSV-associated lower respiratory tract disease by more than 82%, Prakash said.
The most commonly reported side effects of Arexvy are injection site pain, fatigue, muscle aches, headaches and joint stiffness, Prakash added. Ten study participants (out of 12,500 total) who received the vaccine reported atrial fibrillation, Prakash said, but the irregular heartbeat was also reported by four participants who received placebos.
The FDA found the data on atrial fibrillation in relation to Arexvy is “insufficient to determine a causal relationship to the vaccine,” but the company manufacturing it has committed to assessing atrial fibrillation in a post-market study, Prakash said.
Along with adults older than 60, infants and small children are also considered particularly vulnerable to serious RSV outcomes. The vaccines are not currently available to children, but the FDA has approved a preventative antibody for use in children up to 24 months of age.
Signs of different respiratory viruses
While it can be difficult to determine whether you’re experiencing symptoms from COVID-19, RSV or the flu, there is some variation in the indicators.
For example, headaches can be caused by a number of maladies, but are more common in COVID-19 cases than for people who have common colds, according to the Mayo Clinic.
Muscle aches, tiredness and loss of taste and smell are also more frequently seen in COVID-19 cases than in cold cases, the Mayo Clinic reports, and diarrhea and vomiting can be COVID-19 symptoms but are not caused by common colds.

