I was fit and healthy - but had a heart attack at 35

A sharp pain in her wrist woke Clare McStay in the middle of the night. Perhaps she’d pulled something pushing her youngest daughter up a hill in her buggy the day before? Then the dull ache spread to her jaw. She must remember to call the dentist tomorrow, she thought.
But the wrist pain worsened, so with her husband Paul away working in Singapore, she got up and walked around the house in an attempt to ease it — trying not to wake her three children, Sophie, James and Emily (then three, five and eight).
“I unlocked the front door, took the dog out into the drive and dialled 111 for advice. That was the last thing I remembered,” says Clare from Lymington, Hampshire.
The nurse on the other end of the phone called an ambulance, while their family dog woke Emily, to witness her unconscious mother being taken off to hospital.
I’d never smoked, nor been a heavy drinker, I was fit, healthy and active. With three young children and a husband who travelled a lot with work I never sat down
Clare came round in the resuscitation unit at Southampton General Hospital - although she was only 35, she had suffered a massive heart attack. Doctors had fitted a stent after an angiogram revealed one of her coronary arteries had narrowed by 99 per cent.
“I’d never smoked, nor been a heavy drinker, I was fit, healthy and active. With three young children and a husband who travelled a lot with work I never sat down,” says Clare today, two years on.
The angiogram revealed Clare had “ballooning” in her arteries, which doctors attributed to the effects of Kawasaki disease - a rare illness mainly affecting children under the age of five, which has become the leading cause of acquired heart disease in the UK.
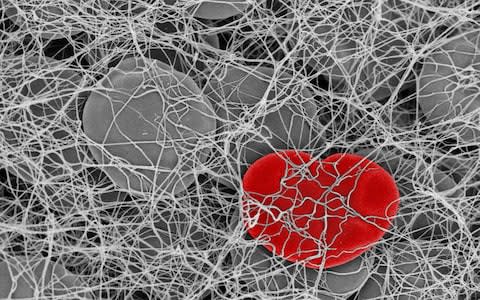
An MRI scan revealed a massive blood clot in her coronary artery, for which she was prescribed a strong anticoagulant (Rivaeroxaban) and asked to return for regular scans and monitoring.
“After one of these on 23 December I was told the clot had gone. In February 2016 I bounced into hospital for another routine angiogram,” says Clare, “Which is where it all went wrong.”
A rare reaction to a chemical called Chlorhexidine, in a disinfectant routinely used on surgical instruments, sent Clare into anaphylactic shock. “I was in horrific pain — more than ever before — and started coughing. I was effectively drowning from the fluid on my lungs (pulmonary oedema) as my heart began to fail.”
Heart failure occurs when the heart stops pumping blood around the body as well as it should. Swelling — usually in the legs — is one of the key signs.
I had no idea these were symptoms of a heart attack — or that I was even at risk of having one. I just want others to be aware
“The body clings on to fluid to try to get more blood pumping,” explains Dr Andrew Flett, a consultant cardiologist and heart failure specialist at Southampton General Hospital. “People with heart failure often feel breathless when walking or lying down flat (when fluid can track into the lungs). This is usually accompanied by other more general symptoms such as lethargy, general malaise, feeling run down and/or poor appetite.”
According to the British Heart Foundation, more than half a million people in the UK have been diagnosed with heart failure. The condition is most common in older people, usually following a heart attack and if an individual has history of smoking, blood pressure and/or diabetes. In young people it is far less common (0.5 per cent of the population under 30).
“Heart failure in younger people is not usually caused by a heart attack but other heart problems such as genetic abnormalities, or if a person’s heart has been damaged through infection, myocarditis,” continues Dr Flett. A common cause in young people is damage through toxins, “which could be chemotherapy or gross excess of alcohol, or recreational drugs such as ecstasy or cocaine.”
Once Clare had stabilised, doctors performed emergency quintuple heart bypass surgery, but warned her husband Paul that her heart was so severely damaged that it might not be strong enough to support her body - only time would tell if she would recover.

After a tense few days unconscious in ICU, with an intra-aortic balloon pump attached to her leg, helping her heart to pump blood around her body, Clare finally came round.
“I had to learn to talk again, and to walk — when you’ve been in intensive care your brain is fried, it needs to recover as much as your body. I was eventually allowed home after a month but I had to adapt my life completely,” she explains.
Achievements in those early days included being able to shower on her own without Paul’s help, to walk down the lane outside the family home, or unload the dishwasher, cook a meal. The McStays live in a bungalow which Clare says has been a “saving grace”, as she doesn’t have to tackle stairs several times a day.
I had to learn to talk again, and to walk — when you’ve been in intensive care your brain is fried, it needs to recover as much as your body
Clare’s heart function is still impaired so she effectively faces an uncertain future — but is determined to do whatever she can to help it strengthen, by living healthily and exercising gently with swimming and walking the dog, as well as remaining hugely positive.
“I am going to see my children grow up,” she says with unwavering conviction. “I know I’ve been very lucky not to get depressed through all this, and I have learnt to say no. I get totally exhausted and it is not a case of mind over matter, I need to stop. I’ve had four or five emergency admissions to hospital for what I call ‘blips’ when my heart has gone into an abnormal rhythm but last November my consultant said he didn’t need to see me again for a year.”
Heart failure is first treated with drugs, including betablockers and ace inhibitors that block the overactive sympathetic nervous system and help to rest the heart by lowering blood pressure and heart rate. Diuretics rid the body of excess fluid and relieve the symptoms.
Women and heart attacks | The warning signs
“Once the condition has been stabilised with medication and the excess fluid has been purged from the system, we recommend cardiac rehabilitation – healthy living and exercise,” says Dr Flett. “If a patient’s heart improves, the prognosis is good, but this only applies to one-third of people. The other two thirds may go on to need more advanced treatments including other drugs, special pacemakers and defibrillators or, ultimately, a heart transplant.
“Predicting who is going to respond to treatment is difficult — whether you’re going to improve is more related to the underlying cause than the age of the patient.”
Clare’s heart is responding to the medication drugs and she remains determined to build its strength. The couple have a new puppy who they are training to be a PAT (Pets As Therapy) dog and are ambassadors for Wessex Heartbeat, who fund the cardiac unit in Southampton and provided Paul with free accommodation at Heartbeat House, opposite the hospital, during their ordeal.
Looking back isn’t something Clare likes to do — “after what happened, I have to look forward” — but she wishes she had heeded the pain in her wrist and jaw straight away. “I had no idea these were symptoms of a heart attack — or that I was even at risk of having one. I just want others to be aware.”
For more information, visit wessexheartbeat.co.uk

