Five mammogram misconceptions: What you should know about annual screening
I have been interpreting mammograms for more than 25 years, and I have heard just about every misconception there is about breast screening. Unfortunately, women sometimes delay or even forgo having a mammogram because of these misplaced concerns. I want to debunk some prevalent misconceptions, especially since we promote breast cancer awareness at this time every year.
When breast cancer is detected at an early stage, a patient has significantly better treatment options, better outcomes, and improved odds of survival. In fact, when breast cancer is found at stage 1, the five-year survival rate is about 99%. This underscores the importance of routine mammography. This year, 297,790 new cases of invasive breast cancer will have been diagnosed in U.S. women, according to the American Cancer Society. About 43,700 women die from breast cancer annually, according to the Centers for Disease Control and Prevention. As a breast radiologist and physician, I find it distressing that many of these deaths might have been prevented by routine screening. Screening is the most reliable way to detect cancer earlier.
Myth 1: I don’t have any symptoms, and breast cancer does not run in my family.
Reality: 75% of women who get breast cancer have no family history of the disease, and one in eight women (13%) will get breast cancer in her lifetime. This is for average risk women. Even though a woman will have many normal or negative mammograms, just having those results as a baseline makes it easier for radiologists to detect and track subtle abnormalities, which can be critical in early intervention. Monitoring is always easier, better, and safer than finding something new. The benefit of previous mammograms is comparison over time, which can spare a woman from additional imaging and needless worry.
Myth 2: My doctor didn’t tell me I needed a mammogram, so I cannot schedule an exam and I am uncertain of when to screen.
Reality: You can — and should — begin screening mammograms at age 40 and continue that routine every year. This is especially true for younger women, for whom the mortality benefits of screening are greater due to longer life expectancy and who often have more family and career responsibilities. If you are over 40, you don’t need a physician referral for screening. You can schedule a mammogram without a note or referral from a physician.
Annual screening is particularly important for Black women, who are 42% more likely to die from breast cancer and have a higher risk of the aggressive type of cancer. Almost every study has demonstrated that starting mammogram screenings at age 40 saves lives.
Myth 3: A mammogram will expose me to radiation.
Reality: The radiation dose from mammograms is very low. For comparison, there is constant background radiation from our planet and sun that we are exposed to every day. The radiation dose from a mammogram is equal to about two months of daily living.
Myth 4: I’ve heard about overdiagnoses and false positives.
Reality: The risk of delayed treatment outweighs the risk of a false alarm. A delayed breast cancer diagnosis is far more stressful than being recalled for further images.
Plus, advanced technology, such as artificial intelligence (AI), is improving cancer detection. Using AI, radiologists have found hundreds of cancers that otherwise wouldn’t have been detected. Without AI, those cancers would have had another year to grow until the next annual mammogram. Remember: when cancer is found sooner, it means more treatment options and better outcomes. AI does not increase radiation or the time spent in the appointment. It is applied after the mammogram to help radiologists detect abnormalities.
Myth 5: If you have dense breasts, you don’t need a mammogram.
Reality: About half of all women have dense breasts. This type of tissue is not abnormal and does not change the screening recommendations. Dense breast tissue can make it more difficult to interpret a mammogram, but studies show that the use of tomosynthesis (3D mammogram) enables radiologists to find more cancers in dense breasts, particularly aggressive, invasive cancers. Ask for a 3D mammogram when you have your annual screening. At Delaware Imaging Network, you can also add artificial intelligence to your mammogram, which performs well with dense breasts. When you have routine screening, your radiologist can better understand your anatomy to determine what is normal for you.
We talk a lot about the fight against cancer, and an annual mammogram is the best action you can take in that fight. Ask about 3D mammography and artificial intelligence when you make your appointment. If you are age 40 or older, or are at high risk for breast cancer, and you haven’t scheduled your annual screening, do it now. If either of these categories apply to you, and you haven’t been screened yet, now is the time to start. Don’t let misconceptions stand in your way.
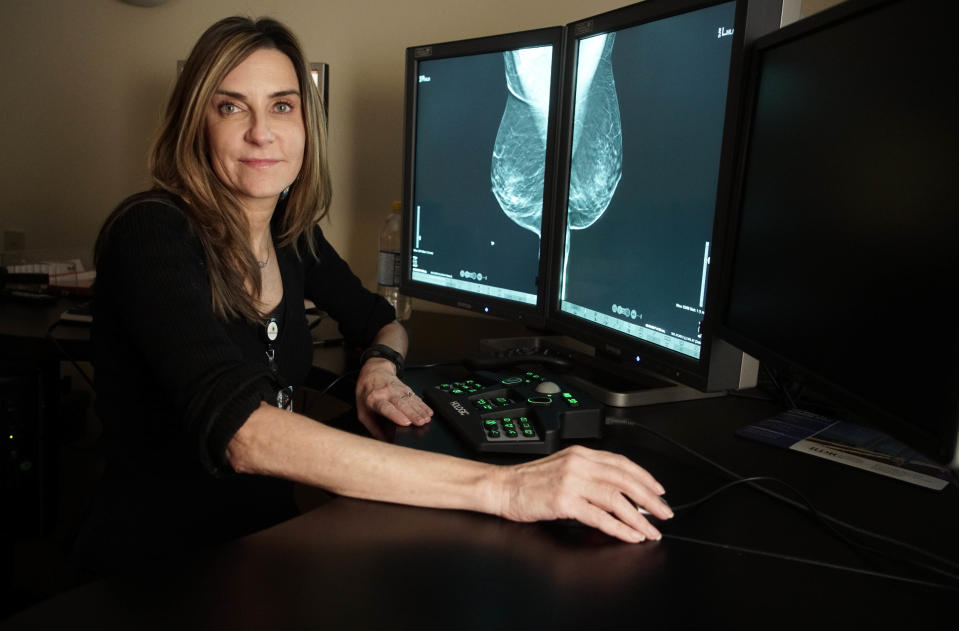
Jacqueline Holt is MD FACR, Medical Director, at Delaware Imaging Network, part of RadNet. For more information about breast health and RadNet’s AI mammogram services, visit https://myebcdmammo.com.
This article originally appeared on NorthJersey.com: Five mammogram misconceptions: What you should know about annual screening

