The Five Phases to Get You a Monkeypox Vaccine
When it comes to monkeypox, there’s good news and bad news.
The bad news: Monkeypox doesn’t look like it’s going away anytime soon. In fact, a rise in cases throughout the United States in recent weeks has stirred concerns (and confusion) from officials at the Centers for Disease Control and Prevention (CDC). At the time of reporting, at least 45 cases of the disease have been reported in states including Arizona, California, Colorado, Washington, D.C., Florida, Georgia, Hawaii, Illinois, Massachusetts, New York, Pennsylvania, Texas, Utah, Virginia, and Washington state, per the CDC.
That might not seem like a lot, but we’re still in the early days of what the World Health Organization (WHO) considers a “multi-country outbreak.” More than 1,200 cases have been reported globally in 29 countries.
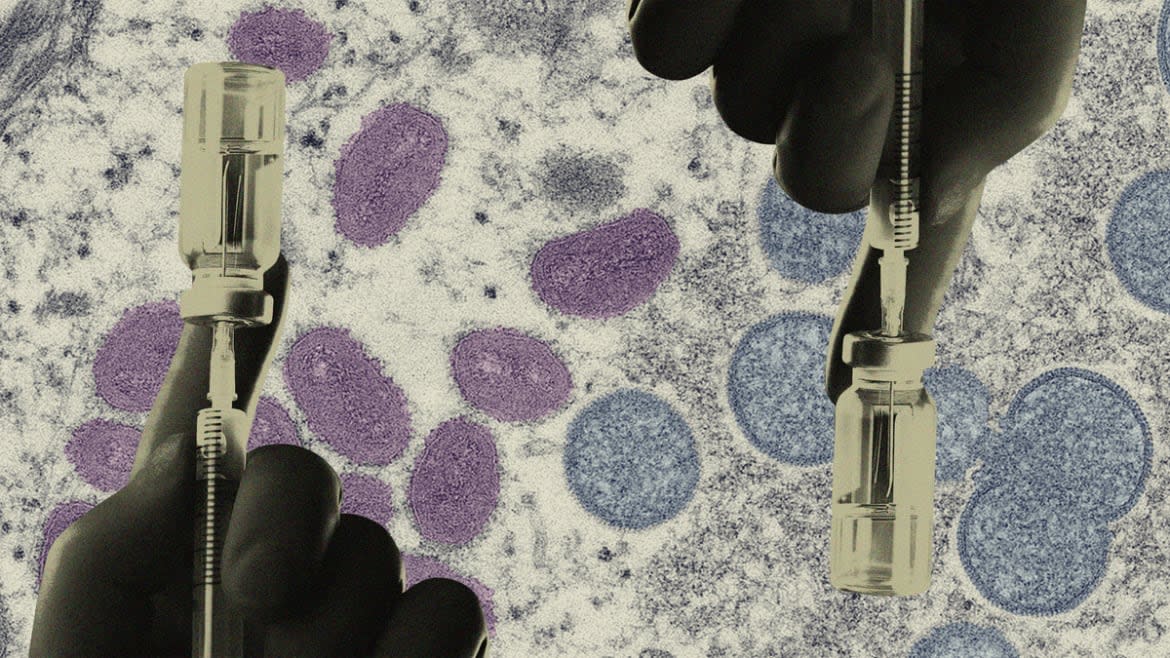
But there’s also good news: We already have a vaccine for it. In fact, we technically have two. That’s because we’ve known about monkeypox for decades now, and since it's a derivative of smallpox, we can even use the smallpox vaccine for it. Heck, we even have effective treatments for it. The White House has even ordered the distribution of 1,200 doses of a monkeypox vaccine to people who have had high-risk exposure to the disease in an effort to nip it in the bud. So even if it does get to pandemic levels of crisis, the world won’t have to wait a year for an effective treatment and vaccine to be developed and distributed like with COVID-19.
Monkeypox is also vastly different from the coronavirus pandemic (which—might we remind you—is still not over). For one, there’s the transmissibility factor: Monkeypox just doesn’t spread as easily as COVID. Yes, there is an incredibly small chance that you can catch it through airborne particles, according to the CDC. However, that isn’t liable to cause the level of cases and deaths that we’ve seen from COVID.
“Relatively speaking, monkeypox is not and will not be that kind of threat,” Iriwin Redlener, a senior research scholar and founding director at Columbia Climate School’s National Center for Disaster Preparedness, told The Daily Beast. “I hope I don’t live to regret these words, but I don’t see how monkeypox can become that infectious and kill that many people like COVID did.”
Of course, that’s a bit of cold comfort for those who have long suffered under pandemic and lockdown anxiety. The fact that there’s a new and, frankly, scary-sounding disease out there that could potentially get out of hand isn’t going to help us sleep at night. However, the fact remains that we’re better prepared for the monkeypox than we were for COVID-19 by a large margin—mostly because we already know how to beat it.
There are currently two jabs we can use to fight monkeypox. The first is called Jynneos, a newer generation vaccine that’s delivered in two doses, and is the CDC’s go-to recommendation specifically for monkeypox. The other is ACAM2000, which is an older smallpox vaccine that can have much more severe side effects, but will still protect against monkeypox.
Should the U.S. Give Out More Monkeypox Vax for Party Season?
Currently, the U.S. has roughly 1,000 doses of Jynneos at hand. The White House could have as many as 2 million doses of Jynneos in reserve, according to a statement from Bavarian Nordic, the Danish pharmaceutical company that produces the shots. The U.S. also has a stockpile of more than 100 million doses of ACAM2000.
As of last week, the CDC has released 500 doses of Jynneos and 200 doses of ACAM2000 to protect vulnerable individuals as well as those who may have high-risk exposures to the monkeypox. If cases continue to rise, though, we might have to enter the uncomfortably familiar scenario of figuring out a large-scale rollout of shots. While the chances of that are very low, we have to be prepared for the worst case scenario, said Redlener, especially after seeing the cracks in the foundation of our current pandemic response systems from the past two years.
To that end, there are roughly five phases that the U.S. would have to nail down in order to ensure a good rollout of a monkeypox vaccine beginning with the stockpile of doses.
The first has to do with supply. One of the biggest reasons the COVID-19 pandemic was so deadly was because we didn’t have a readily available vaccine. Luckily, the U.S. already has a sizable stockpile of monkeypox jabs on hand in case of the worst case scenario. Bavarian Nordic said they have plans to increase production this summer to potentially produce 30 million shots in a year in response to potential demand increase.
Monkeypox Is Spreading During Sex—and That Is Actually a Relief
“I think the stockpile is good,” Redlener said. “To me, if I was looking over the process of preparedness for monkeypox, I’d say we’re in pretty good shape”
The second phase would be to set up a system to test people for monkeypox. The system would need the flexibility to scale up fast if infections increase precipitously.
“We need to build up our testing capabilities, and that includes using the state labs that are already able to test for orthopox viruses,” Brian Garibaldi, the director of the Johns Hopkins Biocontainment Unit, told The Daily Beast. “The CDC has already asked academic centers to think about setting up their own in-house tests, much like we did with COVID. So building that testing capability so that we can very easily test anyone who has a rash that we’re worried about very quickly and easily. That’s going to be key.”
Contact tracing, the third phase, would be similar to our COVID response too. It would be a process of identifying the people who might have come into contact with a person infected with monkeypox. This process is already underway in places like New York City, where there are 10 people who reportedly have monkeypox.
If caseloads continue to rise, we then reach a much more nebulous and uncertain fourth phase: setting up vaccination sites. This will ultimately be determined by where monkeypox is impacting people the most and how accessible it is to vulnerable populations.
“Where do people go to get it? How do they know where to get it? I'm not sure,” Redlener said. He adds that the CDC would likely use traditional medical care sites like hospitals and doctors’ offices to administer vaccines, as well as setting up pop-up vaccination centers like we saw at the height of the COVID pandemic.
Depending on the severity of the disease, we then might reach the fifth and final step of the rollout: aggressive marketing. Redlener said that there would need to be a concerted effort to make sure people know exactly where to get it, how many jabs they need, and what they should expect in terms of the experience and side effects.
Good messaging isn’t just telling people to get the vaccine either. Since the monkeypox seems to be primarily spread through close, physical contact like sex, there could be a stigma attached to it that those infected don’t want to be associated with. We’ve seen this already with diseases like HIV. That embarrassment could become a huge problem when it comes to properly combating this disease.
“We have to be open and honest about identifying cases and making it such that people can come forward and not be stigmatized for having this,” Garibaldi said. “That's number one, because if people feel like they can't safely come forward, then we are going to have cases that don't get reported.”
Plenty of lessons can also be gleaned from the not-so-smooth rollout of the COVID vaccine, where disinformation ran rampant due in no small part to the confused and misleading messaging from bad actors. This, of course, resulted in a cottage industry of anti-vax conspiracy theories.
So, unfortunately, convincing people to actually get the vaccine could prove to be the most difficult part of the rollout.
“I think it would be very tough to convince the American public that they now need to worry about monkeypox to the point where they have to get a special vaccine,” Redlener said. “I think that would be a big challenge. In some ways, the public messaging would be as big or bigger of a problem as the actual distribution of the vaccine.”
Got a tip? Send it to The Daily Beast here
Get the Daily Beast's biggest scoops and scandals delivered right to your inbox. Sign up now.
Stay informed and gain unlimited access to the Daily Beast's unmatched reporting. Subscribe now.

