Following national trends, Florida is seeing a spike in COVID driven by JN.1 variant
For the fourth year in a row, the holidays have brought an increase in COVID cases and hospitalizations to Florida. This trend can be seen throughout the nation, with the new COVID variant JN.1 driving the surge.
As of Dec. 22, the Centers for Disease Control reported that JN.1 — a descendent of the Omicron substrain BA.2.86, which hit the U.S. during the summer — made up 44.2% of all COVID cases in the country.
"At this time, the spread of JN.1 does not appear to pose additional risks to public health beyond that of other recent variants," the CDC said Dec. 22. "(The) CDC is closely monitoring COVID-19 increases domestically and internationally and will communicate if the situation changes."
While the variant appears more immune evasive than others, deaths attributed to COVID for both this winter season and the last have been lower than in 2020 and 2021, though they're still trending upwards nationally. Still, hospitalizations are in the tens of thousands around the nation. In Florida, that number is lower, but sharply increasing.
Here's what the data says.
Hospitalizations, emergency room visits trending up
During the week of Dec. 23, Florida saw an uptick in hospital admissions and emergency department visits attributed to the virus. These factors increased compared to the prior week, while deaths attributed to the virus fell, according to the CDC. Here's how that breaks down:
1.2% of all deaths were attributed to COVID, a 25% decrease
1,391 new hospital admissions of confirmed COVID, a 21.8% increase
1.7% of emergency department visits involved a COVID-19 diagnosis, a 10.8% increase
National data for the same time period:
3.3% of all deaths were attributed to COVID, a 10% increase
29,059 hospital admissions of confirmed COVID, a 16.7% increase
2.5% of emergency department visits involved a COVID diagnosis, a 12% increase
During the summer — when COVID levels last surged — national hospital admissions peaked Sept. 9 at 20,960. They fell to 15,052 on Nov. 4 before beginning to increase again.

Multiple illnesses circulate this winter What are Americans catching this winter? It's not just flu and COVID-19 anymore.
JN.1 symptoms COVID variant JN.1 is nearly half of COVID cases in US, CDC says. What are the symptoms?
How much COVID is circulating in the community?
The CDC reported that for the region including Florida, Georgia, South Carolina, North Carolina, Kentucky, Tennessee, Alabama and Mississippi, 6,124 tests took place during the week of Dec. 23. There was a test positivity rate of 8.6%, an increase of 1.1% from the previous week.
Nationally, the test positivity rate was 12.7% for the week of Dec. 23, an increase of 0.7% from the prior week.
It's important to note not everyone with symptoms takes a test, and at-home tests aren't reported.
Biobot, a company that tracks the presence of diseases in wastewater around the country, showed the national average of COVID-19 viral concentration in wastewater was 997 per milliliter as of Dec. 23. That's just slightly below last year, when the company recorded a concentration of 1,086 copies per milliliter on Dec. 24, 2022.
The 2022-2023 winter surge peaked on Dec. 31, 2022 with 1,160 copies of COVID-19 per milliliter of wastewater.
Small percentage of the nation vaccinated
As of Dec. 9, only 18.3% of adults reported having received their 2023-2024 COVID shot on the National Immunization Survey despite the vaccine being approved several months ago, the CDC reported. The statistic for children ages 6 months to 17 years was even lower, with parents and guardians reporting that only 7.8% of their children had received a shot.
Vaccines are available at most pharmacies, though some require an appointment ahead of time.
Pfizer-BioNTech and Moderna vaccines are available for everyone 6 months old and above, while the Novavax vaccine — currently the only COVID-19 vaccine in the U.S. that does not use mRNA — is available for everyone age 12 and older.
While the CDC maintains that all three COVID vaccines are safe, Florida Surgeon General Joseph Ladapo has called mRNA vaccines into question multiple times. On Wednesday, he called for the FDA and CDC to stop the use of mRNA vaccines in humans, citing safety concerns about "nucleic acid contaminants."
Even with the newer variants, vaccines help reduce the risk of severe illness, hospitalization and death. However, the "protection against infection tends to be modest and sometimes short-lived," according to the CDC.
Testing and treatment: How to test and where to get treatment
While the CDC recommends testing immediately if you have symptoms, a study published in the journal Clinical Infectious Diseases suggested that testing on the fourth day of symptoms may produce the most accurate result. In the study, researchers examined 350 people with COVID and found that their viral load peaked four to five days after symptoms started.
If you don't have symptoms but have been exposed, you should wait five days before testing, according to the CDC. If you are using rapid tests and receiving negative results, you should test twice more with 48 hours between each test, as negative results are not always accurate. A positive result is reliable.
PCR testing generally only requires one test and is the most accurate test available. However, it's no longer free in most cases due to the federal emergency ending in May of last year, and not all insurances cover COVID tests.
Some Walgreens locations have free at-home PCR tests through Labcorp that do not require insurance. Check to see if your Walgreens offers these tests by visiting their website.
Rapid tests are sold at pharmacies and grocery stores. The federal government offers p to four free tests per household on the Department of Health and Human Services website.
Paxlovid is generally prescribed through your primary care physician, an emergency department or urgent care, online telehealth or pharmacists if you test positive.
My symptoms are mild: Why test?
While estimates vary, the CDC reported in summer 2022 that approximately one in 13 American adults were suffering from long COVID, a condition with a variety of symptoms including fatigue (especially after any kind of exertion), brain fog, chest pain and more. Out of the general population who had previously had COVID, they estimated about one in five had long COVID, with people of color and LGBTQ populations at an increased risk of developing the condition.
Those with long COVID advocate for testing so there's documented proof of infection in case you need to seek treatment for long COVID in the future.
Testing can also help rule out a COVID infection and help you decide if you want to seek testing and treatment for the flu, RSV or bacterial infections.
I'm sick. How long do I have to isolate?
If you're sick and think it might be COVID, the CDC recommends isolating at home for at least five days and wearing a high-quality mask if you have to be around other people. If you are fever-free after five days and other symptoms are improving, you can end isolation. However, you should still wear a mask indoors and avoid being around high-risk individuals for at least 11 days.
If you had moderate symptoms such as shortness of breath, or you have a weakened immune system, the CDC advises isolating through day 10.
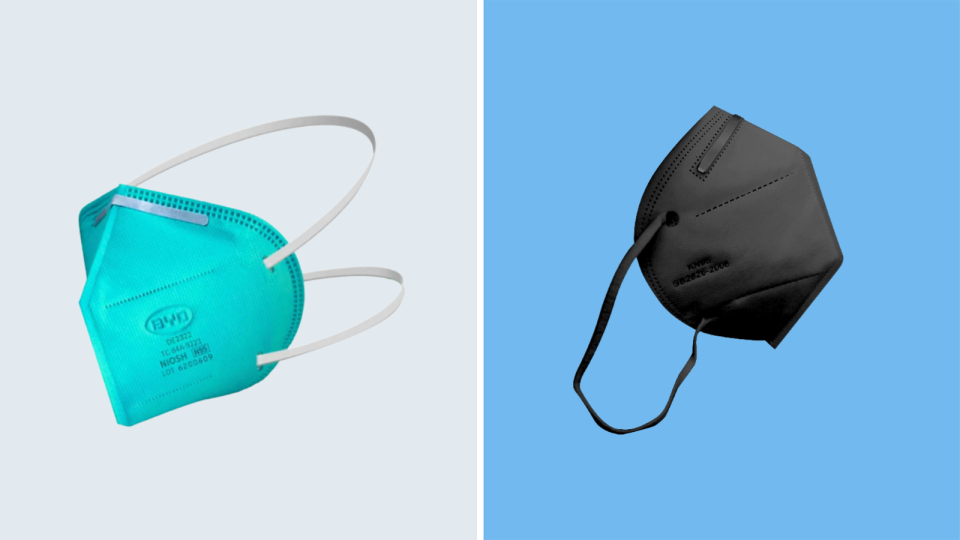
Because schools and employers have dropped COVID-19 policies, not everyone can isolate while sick. If you need to be around people, the CDC recommends wearing "highly protective mask or respirator," like a KN95 or N95. These masks can generally be purchased at home improvement stores, or may be available for free through links listed on the CDC's website.
Finch Walker is the education reporter at FLORIDA TODAY. Contact Walker at fwalker@floridatoday.com. X: @_finchwalker.
This article originally appeared on Florida Today: COVID is on the rise in Florida: Here's how to protect yourself

