Former Tory MEP reveals how she was put under DNR order against her will

- Oops!Something went wrong.Please try again later.
A former Tory MEP has told how she was given a “do not resuscitate” order at the height of the pandemic without her consent or even her knowledge.
Caroline Jackson, 74, a former chair of the European Parliament’s Environment, Consumer Protection and Public Health Committee, was admitted to John Radcliffe Hospital in Oxford last May for an operation on her broken pelvis.
However, she was “very shocked” to discover after her discharge that medics had decided she should not be resuscitated in the event her heart stopped.
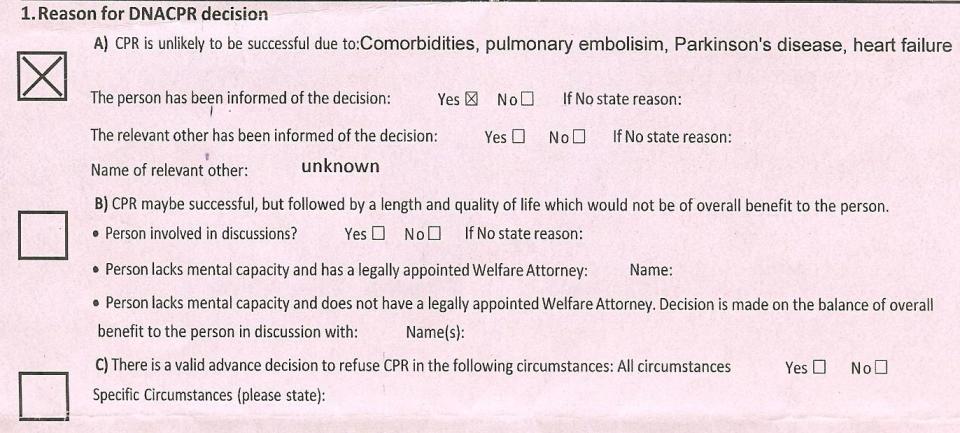
A DNR form in her notes stated, via a series of tick boxes, that she had been informed of the decision, which was authorised by a consultant, and that the order was in place on an “indefinite” basis.
Neither Mrs Jackson nor her husband have any recollection of the matter being discussed.
“I had no opportunity to be asked about it, to consider it myself. My husband knew nothing whatsoever about it,” she said.
Mrs Jackson’s case will stoke fears that DNRs have been applied too readily during the pandemic, and will raise questions over whether doctors were under pressure to apply them in order to ensure that the NHS did not become overwhelmed.
Blanket use of DNRs
The NHS has repeatedly written to Trusts to make clear that the blanket use of DNRs is unacceptable.
However, a Telegraph investigation has found that some medics have decided that patients with mental illness and learning disabilities should not be resuscitated if their hearts stopped.
Now, Mrs Jackson, a historian, has called for an overhaul of the “tick box system” used to regulate DNRs, warning that there is a “very real danger” of them being applied to patients without their or their family’s involvement.
It is “not a procedure that should become automatic and regulated only by a tick box system”, she said.
Clearing patients
The procedures should be examined as part of official reviews into how the NHS coped with the pandemic, Mrs Jackson said.
“It's not just a question of the obvious things like, who gets the jab…but it's what happens in the hospitals, when, for example, we try to clear the patients in order to create space for victims of the pandemic.”
Her own ordeal began in April last year when she tripped on a rug at home, three weeks into the first lockdown. She suffers from Parkinson’s and has regular falls, and initially thought little of it as she was still able to go on long walks.
However, after a few weeks of worsening pain, doctors found that she had broken her pelvis and she was admitted for her emergency operation. She initially had a problem with a pulmonary embolism, but otherwise made a strong recovery and was discharged after 17 days.
Mrs Jackson did not discover the DNR that had been applied until a few months later when she was sorting through her hospital notes.
Ticked box
“I saw a lilac form, which I now know to be a do not attempt resuscitation order, with my name at the top. I still don’t know whether they meant me to take it away, but I was shocked, very shocked, to see a cross in a box at the top of the form indicating that I was not a candidate for resuscitation in the event that my heart stopped,” she said.
It had not occurred to her before that she could be a candidate for a DNR.
“I am a 74-going-on-31-year-old retired member of the European Parliament, and was just keen to get home to my husband, friends, and my regular Pilates classes.
“At no stage had the DNR been discussed with me or my husband. Nor do I have any recollection of discussing the matter, or even meeting, the doctor who apparently signed it off on 20 May, four days after my surgery.”
Mrs Jackson has since written to the head of the hospital with her concerns, calling for a review of the way that the consultations around DNARs are carried out.
People are unaware
“I can't believe that I'm the only person in this position who was designated as DNR, and who wasn't mentally deficient. I suspect that there are quite a lot of these little lilac forms lying dormant in people's files. Many people may still be unaware they were given such orders.”
She has also raised concerns over the rationale behind the decision. According to the form, cardiopulmonary resuscitation (CPR) was unlikely to be successful for a number of reasons including her Parkinson’s disease.
According to the charity Parkinson’s UK, being diagnosed with the disease “is not in itself grounds to make a DNR decision”.
"Where there is doubt about the significance of the comorbidity, we believe it is good practice for the clinician making the resuscitation decision to discuss it with the patient's specialty consultant if possible," added Rowan Wathes, an associate director of the UK Parkinson's Excellence Network.
End of life wishes
Mrs Jackson said her hospital stay offered her some insight into how DNRs might sometimes be applied without proper consultation.
She recalled a nurse going from bay to bay asking patients about their end of life wishes, and being unsettled by a discussion she overheard.
“She asked words to the effect of, ‘this is a very difficult question for us to consider, but do you have any thoughts about what you would like to happen if the operation is not successful, and further operations are needed?”, Mrs Jackson recalled.
“I remember being unsettled by the answer from one of my elderly neighbours, who said 'Oh my dear I’m going to have to leave that to you. Whatever you say is in one ear out the other. I’ll leave it to you'."
Professor Meghana Pandit, chief medical officer, Oxford University Hospitals NHS Foundation Trust, said on Friday night that it regularly audits DNR decisions to ensure they are made in line with guidance.
“All staff are trained to come to a judgement on treatment, including end of life care, in discussion with their patient and in a way that is compassionate and informative, as well as in line with national guidance, which is clear there should be no blanket application of these instructions,” she said.
DNR orders, the pandemic, and protecting the NHS
When Dominic Cummings released a picture from inside Downing Street at the start of the pandemic of a whiteboard showing the words, “who do we not save?”, it threw into sharp focus the enviable dilemma faced by the Government of trying to treat patients whilst ensuring the NHS could cope with Covid-19, Claire Newell writes.
Who – if anyone – were they willing to sacrifice?
One potential answer to that question emerged last year, when it was reported that thousands of elderly people were denied potentially life-saving treatment to stop the health service being overrun.
Intensive care doctors told the Sunday Times that documents containing triage criteria – which gave a score for age, frailty and illness – were used in hospitals in Manchester, Liverpool, London, the Midlands and the southeast.
NHS chiefs responded by disputing that the elderly were abandoned, saying it was “demonstrably wrong”.
“The NHS repeatedly instructed staff that no patient who could benefit from treatment should be denied it and, thanks to people following Government guidance, even at the height of the pandemic there was no shortage of ventilators and intensive care," they said.
But they did admit that they were asked to look at devising a “triage tool” and the Department of Health and Social Care admitted the existence of the guidance when they said it was never formally published.
The Telegraph’s investigation into “do not resuscitate” orders now offers another potential explanation as to how care appears to be restricted during the pandemic.
This week, we revealed how patients with mental illness and learning disabilities were given the orders – known as DNRs (or 'do not attempt cardiopulmonary resuscitation') – and now, we are able to tell the story of a former MEP who said she was given such a decision without her knowledge.
DNRs are only supposed to be put in place with the agreement of the person concerned or, if they lack the mental capacity to do so, following a discussion with their next of kin.
Doctors do not need to obtain consent, but many forms ask whether the patient or their family has been told, and that is generally considered best practise.
In the case of Caroline Jackson, the documentation in her file asks whether the “person has been informed of the decision” and “yes” is ticked – despite Mrs Jackson saying she was unaware.
Having a DNR in place means that doctors will not attempt resuscitation of a patient’s heart stops.
They avoid putting those who are near the end of their lives already through the distress of a resuscitation when their quality of life and chances of long-term survival are very low.
Yet, it seems unlikely that Mrs Jackson would have fit into that category, which raises the question about why it was given at all.
Matt Hancock, the Health Secretary, has been adamant that everyone who needed care during the Covid-19 crisis received it, but these revelations challenge this view and raise the possibility that some medics may have taken it upon themselves to decide who would receive care and who would not by using these “orders”.

