Freedom for Fingers
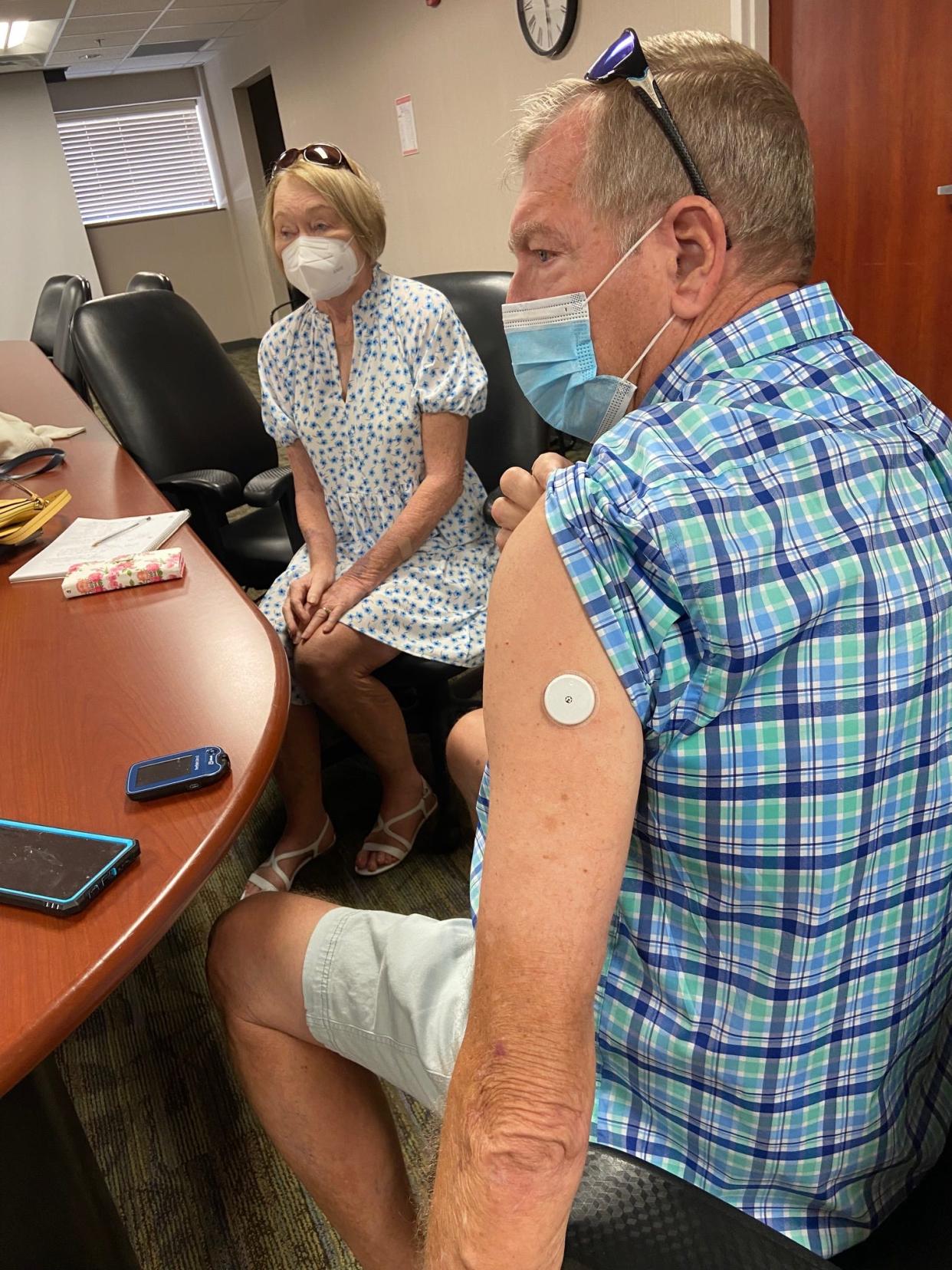
Jerry Branham, a competitive shuffleboard player, is among the many diabetics who use continuous glucose monitoring to check their glucose levels instead of needing to do multiple finger sticks each day.
“Continuous glucose monitoring is convenient,” the Lakeland-area resident said. “I can check my sugar as many times as I want.”
How does he check it?
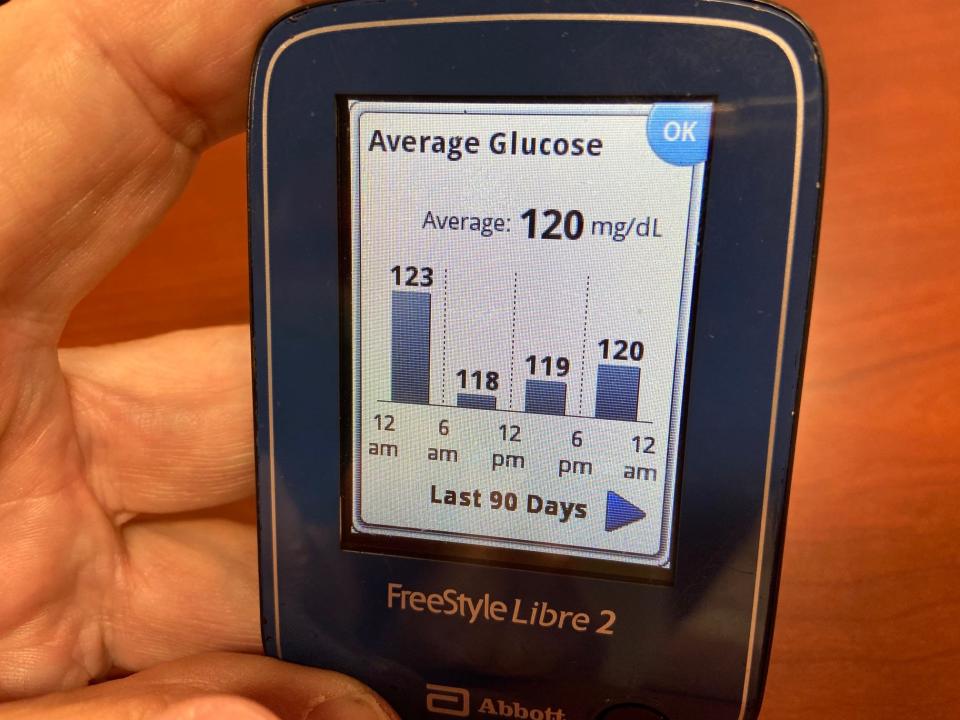
By looking at the screen of a reader small enough to tuck in his pocket.
It can show his body’s current glucose (sugar) level and trends like his average level over the past 90 or 120 days.
That’s preferable to feeling slightly shaky on the shuffleboard court, or in his younger days the softball field, when he did finger-stick monitoring.
That would have meant stopping play and finding his glucose monitor to check his level.
The CGM sensor on his arm is about the size of two quarters stacked.
Debbie Branham, his wife, also switched to continuous glucose monitoring. Her CGM system sends readings to her insulin pump.
Diagnosed at age 3, she has type-1 diabetes, in which the body isn’t making insulin.
“It makes life so much easier,” she said, demonstrating how the pump and CGM monitor attach to the same leg.
Like her husband, she can check the level as often as she wants.
Jerry Branham’s level was 99 when he checked it at an August interview. An arrow pointing sidewise told the 74-year-old his blood sugar was stable.
The arrow would have pointed up if his level were rising, he said, and pointed down if his level were going down.
Diagnosed with diabetes almost 40 years ago, Branham said he is on insulin injections and another drug to lower blood sugar.
The couple, both Kentucky natives, rely on CGM measurements for daily reassurance and help in planning their food intake.
“Menu planning is one of the biggest things and making decisions on simple things like pizza,” said Debbie Branham, 72.
They do periodic finger stick checks to make sure their CGM systems remain accurate.
The traditional finger-stick measurement checks blood sugar level.
Continuous glucose monitoring checks interstitial glucose, the level found in fluid between the cells.
A sensor attached to the body tests glucose level every few minutes, typically about every five. A transmitter wirelessly sends that information to a monitor, which can be a reader like Jerry Branham has or, for some, a smart phone.

“We’re seeing explosive benefits for patients to be able to track the changes in their blood sugar based on their behaviors,” said Gloria Willey, certified diabetes care and education specialist at Lakeland’s Watson Clinic.
She and four Polk County physicians interviewed strongly support continuous glucose monitoring.
“It’s a good thing for the patients because they know what their blood sugar is all the time,“ said Dr. Erjola Balliu, an endocrinologist with Lakeland Regional Health.
Knowing their levels on an ongoing basis can reassure elderly patients who fear their blood sugar will get so low that it leads to falls, Balliu said, adding, “People are more likely to take their medication because they are not afraid.”
It gives them more confidence about exercising, said Dr. Jessica Castellanos, a Bond Clinic endocrinologist in Winter Haven and Davenport.
“The fact that we are able to see their sugar in real time is a great advancement in patient care,” Castellanos said. “It’s empowering patients.”
Patients aren’t the only ones becoming more informed.
“The fingerstick glucose check just gives a glimpse of what the blood sugar is at that moment,” said Dr. Vindya Boelke, the Watson Clinic endocrinologist treating the Branhams.
Information recorded and stored by the CGM system is more complete, she said, letting patients and their doctors detect patterns and trends.
Continuous glucose monitoring originated for type-1 diabetes, but research expanded its use to type-2 diabetics, particularly those on insulin.
“CGM serves an increasingly important role in managing the effectiveness and safety of treatment in many patients with type-1 diabetes and selected patients with type-2 diabetes,” says a summary of American Diabetes Association 2022 standards of medical care.
The American Association of Clinical Endocrinology strongly recommends it for all people with diabetes treated with intensive insulin therapy and says CGM may be recommended for type-2 diabetics on less intensive insulin therapy.
Boelke said she would recommend it for all but a few patients with diabetes. Balliu and Willey recommend it for most diabetic patients, not limiting it only to diabetics who are on insulin.
Dr. Cara Nelson-James, medical director for countywide Central Florida Health Care, said she recommends it for type-1 or type-2 diabetics who take multiple daily insulin injections
“Many patients come in asking for it because they hate doing finger sticks,” Nelson-James said. “The insurance often times will not approve if the patient isn’t on insulin.”
The other doctors said most of their patients know about continuous monitoring and often ask for it.
Willey still encounters many who don’t understand it.
Some have been told it’s too expensive, Willey said, but she added that with some brands it isn’t much more expensive than monitoring strips for blood checks done several times a day.
Dexcom, the brand Debbie Branham uses, has gone through several upgrades since its first model came out more than 15 years ago. Her sensor is changed every 10 days.
Her husband uses FreeStyle Libre, a more recent entrant that Willey said is less expensive than some others. His sensor goes for 14 days.
Eversense, another CGM system, is designed to last 90 days before changing. Unlike the others, it’s implanted under the skin.
Patients can discuss the pros and cons of different methods and brands with their doctors and with certified diabetes educators.
Contact Robin Williams Adams at robinwadams99@yahoo.com
This article originally appeared on The Ledger: Continuous glucose monitoring replaces finger sticks for diabetics

