Getting COVID-19 Could Weaken Your Immune System
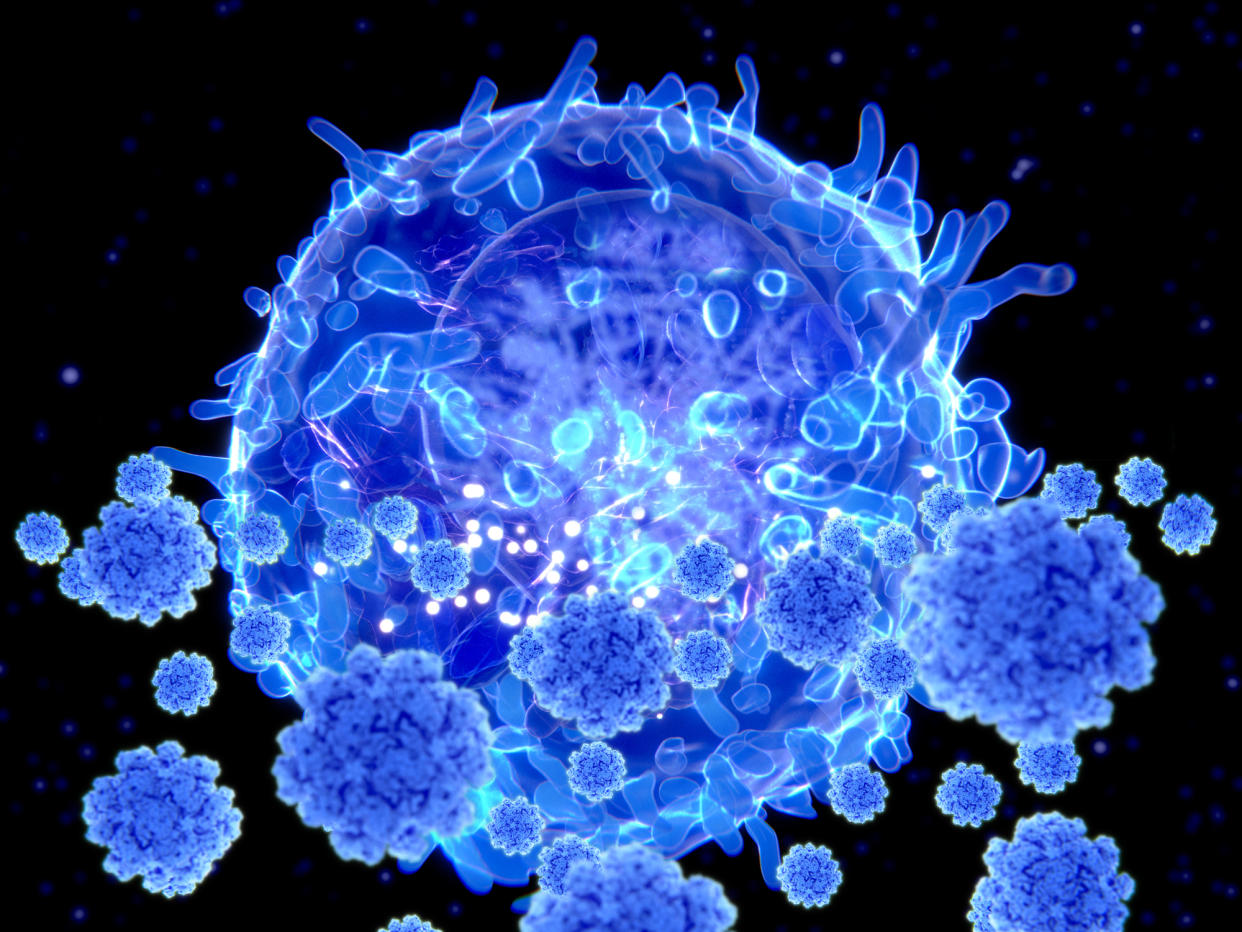
Illustration of a T cell targeting SARS-CoV-2 particles. Credit - Science Photo Library—Getty Images
Even relatively easy bouts with COVID-19 can still take a toll on the immune system, according to a paper published Mar. 15 in the journal Immunity—particularly on T-cells, which provide long term and durable protection against viruses.
Mark Davis, a professor of immunology at Stanford University and director of the Stanford Institute for Immunity, Transplantation, and Infection, and his team made the discovery when studying T cell responses to SARS-CoV-2 among 72 people through the early months of 2021, as the first COVID-19 vaccines were becoming available. They used the most sensitive method available to track changes in T cell responses, relying on an engineered molecule that can detect up to five-fold more T cells targeting SARS-CoV-2 than other molecules. The researchers focused on three groups of people: those who were not yet vaccinated and had gotten COVID-19, those who were fully vaccinated with two doses of the Pfizer-BioNTech mRNA vaccine and had not been infected, and people who had gotten vaccinated after recovering from COVID-19.
The researchers looked at a group of T cells called CD8 cells, or killer T cells, which destroy and remove infected cells during the latter part of an infection. Davis was surprised to find that levels of CD8 cells were lower among people who had gotten vaccinated after recovering from COVID-19, compared to those who had been vaccinated and never infected. The results differ from changes in antibodies, which are the body’s first line of defense and help block viruses from infecting cells. Studies of COVID-19 patients show that antibody levels in people who have been vaccinated and infected tend to be slightly higher than levels of antibodies among those who have been vaccinated and never been infected—creating hybrid immunity. The opposite was true with CD8 cells. “Sometimes you do experiments and don’t always know what you’re going to get, and something jumps out at you, and that was the case here,” Davis says. The fact that they saw “dramatically lower CD8 or killer T cell responses than everyone else” indicated that “there was some damage—something was happening after the infection in these people.”
More from TIME
Read More: How COVID-19 Changes the Heart—Even After the Virus Is Gone
Because researchers took multiple blood samples from the volunteers over the four-month study, they were able to delve deeper in how the T cell populations were changing, and confirmed the pattern. Vaccinated people who had not had COVID-19 generated CD8 T cells up to 67.1-times higher than they did before they got the shots. While people who had recovered from COVID-19 and then got vaccinated also produced higher levels compared to baseline, these were anywhere from 3.6- to 54-times lower than the levels generated by the first group. “It turns out the virus suppresses CD8 responses,” says Davis. “It could be making it more difficult for CD8 cell populations to come back up again.”
“The message is that with this disease, we are not completely out of the woods yet when the virus is gone,” says Davis. “We generally think in terms of the T cell response that more is better, so what we saw in the reduction in the number of cells can’t be good.”
Researchers don’t yet know what a weaker CD8 response against SARS-CoV-2 means for a person’s health. But the study also showed that people in this group still benefited from the vaccine—just not as much as those who hadn’t been infected before getting it. Levels of CD8 cells among those who had infections and then were vaccinated were still higher than levels among unvaccinated people.
The results raise the question of whether the apparent damage to CD8 T cell production might contribute to a greater risk of Long COVID, but more data are needed to explore that possibility. “There can be lasting damage that might be resulting in something like Long COVID, or it might be something else,” says Davis. “We don’t know yet.”
Given these findings, can repeated COVID-19 infections continue to dampen the T cell response, and increase the likelihood of Long COVID or worsening symptoms? It’s possible, since experts believe that the T cell response is responsible for the more durable protection that keeps people from experiencing severe disease resulting in hospitalization or death. But that question, too, remains unanswered.
These results, which shed light on how T cell immunity responds to natural infections and vaccines, should play a role in ongoing discussions about booster shots, says Davis. Another key will be studying whether the same pattern is found with other types of COVID-19 vaccines that don’t rely on mRNA. He and his team also looked at CD4 T cells, or helper T cells, which work with antibodies soon after infection to block as many viruses from infecting cells as possible. They found that, unlike with other vaccines against viruses, the CD4 and CD8 T cell responses are not synchronous after immunization. Normally, both populations of cells rapidly increase in response to a vaccine, but after the Pfizer-BioNTech shot, levels of CD4 cells rose first, while CD8 cells didn’t peak until two weeks later. Davis suspects that may be related to the mRNA vaccine formulation and the way the mRNA shots present the viral targets to the immune system.
“We hope that with this study, people will look at some of the more recent vaccine formulations, not just mRNA,” he says, to gain more knowledge about which formulation might produce the strongest T cell response. As more and more people get infected, “the best impact of this would be to stimulate further investigations to see if we can boost those CD8 T cells.”

