Hanif nearly died from a sickle cell crisis at age 8. Now cured, he's headed to Harvard
VALHALLA — At age 8, Hanif Mouehla lay unconscious, intubated in Maria Fareri Children's Hospital as his small body fought through another sickle cell crisis.
Now 17, Mouehla is heading to Harvard. He graduated from Northern Valley Regional High School in Old Tappan, New Jersey, in June — while there, he served as class president, established the school's Black Student Club and played Varsity football.
Mouehla plans to major in molecular and cellular biology on a pre-med track. He wants to specialize in hematology, the study of blood and blood disorders like sickle cell, the disease that nearly killed him and the one that a research treatment cured.
Yes, Mouehla is considered cured.

In October 2014, Hanif received a stem cell transplant from his mother, with cells customized to be more resilient and compatible to him, using cellular engineering. The process is the subject research study led by Dr. Mitchell Cairo, section chief of pediatric hematology, oncology and stem cell transplantation at Maria Fareri, part of Westchester Medical Center.
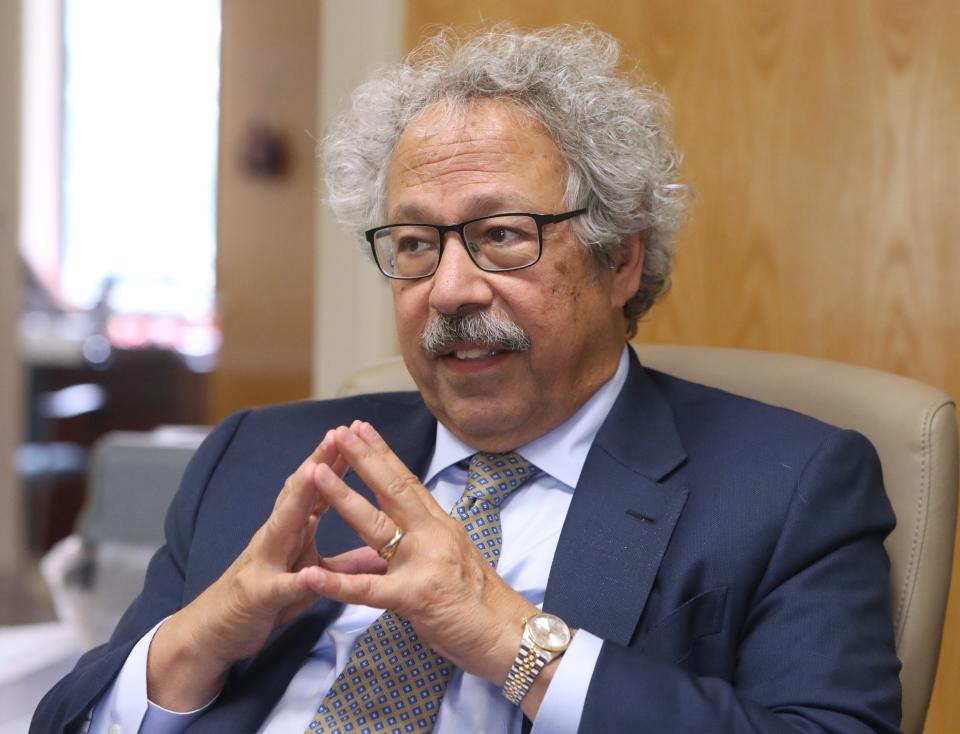
"We've changed a chronic disease into a curative disease," Cairo said.
Khuraira Musa, Hanif's mom and his donor, framed the treatment as the key to the future.
Before the breakthrough treatment, Musa's dreams for her youngest son were limited to hoping he would be safe. "We didn't have the luxury to dream beyond that," Musa said, let alone think that one day he would be heading off to Harvard.
'You can do anything you want'
By third grade, Hanif Mouehla has already suffered significant health consequences from sickle cell. He was smaller and less energetic than most kids. On hot or cold days, he would sit at the window and watch his brothers, Kamil and Jamil, play outside.
Hanif's brothers, twins and two years older, didn't have to worry about overheating or getting too chilled and setting off a sickle cell crisis like Hanif. They didn't have to battle the fatigue chronic anemia brought.

Hanif's last attack, the one that left him unable to walk in its wake, happened when he was a third-grader at Grandview Elementary in the East Ramapo school district.
It was torture for his mother to watch.
From NICU baby to baby doctor: How hard work, mentorship led man to med school and beyond
But that lengthy hospitalization that put little Hanif's life on edge led to Cairo's intervention.
Musa recalls a doctor she didn't know, coming to her son's bedside multiple times, checking machines and charts.
Then Cairo introduced himself. He told Musa about the study that WMC was leading, with hospitals participating around the nation. He explained how genetic engineering could create a bone marrow transplant match that could permanently wipe out her son's sickle cell.
It came with risks, and even could be fatal, Cairo explained. But it also could mean a cure and a chance at a future.
"I just trusted him," Musa said during a recent visit with the doctor. "He had such a nice energy about him."
Cairo recently reflected on the sickly little boy he saw a decade ago, the young man who now towers over him as he gives his doc a bear hug when they meet. By the time Cairo was brought into young Hanif's care, the youngster had already suffered from one of the most serious side effects of sickle cell — acute chest syndrome, which damages lungs and can lead to other organ damage and death. "That is a bad sign of worse to come," Cairo said.
Now, what does the future hold for Hanif Mouehla?
Cairo looked over at his former patient as he answered: "You can do anything you want."
90% in trial are disease free
Cairo heads the familial stem cell transplant clinical trial at Maria Fareri Children’s Hospital, which is the lead center of hospitals across the country participating in study of transplants using re-engineered donor cells.
The work is done at Westchester Medical Center's Cellular and Tissue Engineering Laboratory, which Cairo leads and where Mouehla participated in an internship.
The sickle cell cellular engineering trial is now in the second phase. About 20 participants took place in the first round, with more than 90% of Phase 1 trial participants disease-free one year after transplant.
Phase II, now underway, has about 20 participants and Cairo said he's looking for more. (More information at https://www.mariafarerichildrens.org/sickle-cell-disease or call 914-614-4270.)
Patients from childhood to age 35 qualify. Cairo explained that the younger patients are likely to face fewer complications because they were likely to have less organ damage from past sickle cell crises.

The treatment uses graft engineering to tailor a bone marrow match so it is less likely to be rejected and more likely to create an environment that erases sickle cell. Often, the therapy uses donor blood and marrow from a parent.
Cairo explained: "We took mom's blood cells. We engineered cells to take out certain cells that would cause complications and enriched the population of the most important (cells)."
While bone marrow transplants are used to treat children with sickle cell, finding a perfectly matched donor, usually a sibling, is rare.
About 85% of children with sickle cell haven't been able to access or find relief with current treatments, including traditional bone marrow transplants.
Like a direct bone marrow transplant, the engineered transplantation process can lead to fatal complications in a small percentage of cases.
"Everything is a risk-benefit," Cairo said. But the engineering done to donor cells "significantly ratchets down the risk."
What is sickle cell?
Sickle cell disorder is hereditary. Both parents have to be asymptomatic carriers, commonly called "having the trait," for the disease to show up. The general odds are 1 in 4 of passing on either sickle cell disease or having a child without the trait. Parents who both have the trait have a 50% chance of passing on the trait to an offspring.
But statistics and genetics are tricky. For example, Musa said both she and the boys' father have the trait; the twins do not, even though they faced a 50/50 risk, so they are not carriers; Hanif, with a 25% chance of having sickle cell, was born with the disease. Although he is now free of sickle cell, he does have the trait and could pass it on, said Cairo.
During a sickle cell crisis, red blood cells that deliver oxygen throughout the body clump together and change shape, like a slivered moon, or banana, or a sickle.
That impedes blood flow and it's extremely painful.

Crisis severity varies. A episode can cause organ damage and even death. People with sickle cell disease have a life expectancy of about 54, more than 20 years lower than average. But a serious crisis could prove fatal at any age.
NY hospitals: Some nixed medical debt lawsuits. Others sued 1,600 patients for $9M
Day-to-day life poses challenges. People with sickle cell often have anemia, leading to fatigue. Repeated crises mean more chance of organ damage, including neurological issues.
About 100,000 people in the U.S. have sickle cell; most people with the disease are of African lineage, though people with Hispanic, South Asian, Southern European and Middle Eastern ancestry are also at risk.
Nancy Cutler writes about People & Policy for lohud.com and the USA Today Network New York. Follow her on Twitter, Instagram and Threads at @nancyrockland.
This article originally appeared on Rockland/Westchester Journal News: He almost died of sickle cell at 8. Now cured, he's off to Harvard

