Health care providers take a van to rural Vermont to curb hepatitis C
Three Massachusetts health organizations have embarked on a clinical trial to try to reduce the prevalence of hepatitis C connected to drug use in the rural communities of Vermont, New Hampshire and Massachusetts.
The Rural New England Health Study — a joint effort involving Better Life Partners, Baystate Health and Tufts University School of Medicine — is currently operating in areas around Brattleboro and Keene, New Hampshire, using a van equipped with medical staff, blood testing and syringe services to reach out to people who inject drugs, and might be infected with hepatitis C.
Hepatitis C Virus, or HCV, is among the most commonly reported infections in Vermont, according to Dan Daltry, infectious disease program manager for the Vermont Department of Health. Daltry said more than 800 cases of the disease are identified each year.
"What is problematic is knowing what is acute, what is chronic and what could be historic," Daltry said. "We are working to improve our surveillance."
People can live with hepatitis C for decades without knowing they have it, according to Dr. David de Gijsel, chief health officer at Better Life Partners, who added that hepatitis C is a blood-borne virus that only lives in humans.
"The only way to get it is to get in touch with the blood of someone with hepatitis C," De Gijsel said. "It has to get into your bloodstream. In the United States, the majority of new infections is by sharing needles."
Dr. de Gijsel said about one third of those infected with hepatitis C "clear the virus" through their immune systems, but about two thirds will continue to be infected by the disease, and will live with it for the rest of their lives, if they don't receive treatment.
"Some will go on to slowly destroy their liver, a scarring of the liver called cirrhosis," de Gijsel said. "Once you reach that stage, the only way out is to get a transplant."
New drugs are a 'game changer'
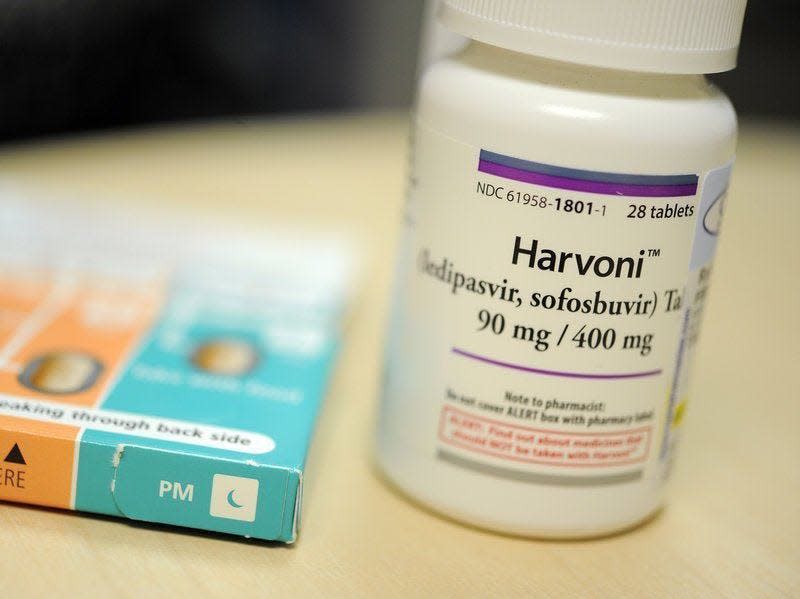
New drugs have revolutionized treatment of the disease, according to de Gijsel. Until about five years ago, treatment was "pretty toxic and very lengthy," up to a year, and only had a success rate of about 50%, de Gijsel said. The new drugs, such as Harvoni, are well-tolerated pills taken for eight to 12 weeks and have up to a 98% success rate.
Dr. de Gijsel said the new drugs are "game changing," and could lead to the elimination of hepatitis C.
"There's no vaccine, but if we treat everyone likely to spread the virus, no more hepatitis C," he said.
The medical community already knew from research that to provide that treatment to active drug users, "you need to leave the hospital."
"It's difficult to engage in traditional health care for a million reasons," de Gijsel said. "Going to the hospital is traumatizing and stigmatizing. Many people had bad experiences."
To make it easier for drug users and others to access treatment, de Gijsel and his team settled on a van equipped to test and treat patients.
"The van parks outside community places where people use syringe programs," de Gijsel said. "We invite them into the van, and offer hepatitis C testing. While they're there, we offer Narcan, clean syringes and engage in conversation."
For those who test positive for hepatitis C, de Gijsel and his team draw a full set of labs to see if a patient is actively infected with the disease. Those who are actively infected are included in the randomized trial, either receiving treatment in the van or being referred to Dartmouth Medical Center or the University of Vermont Medical Center for treatment. The trial will measure the difference in effectiveness of making referrals for treatment or treating patients from the mobile setting of the van.
"You might say, 'Why would you need a trial, it seems obvious people on the van will do better?'" de Gijsel said.
The trial is intended to demonstrate the effectiveness of mobile treatment of drug users infected with hepatitis C — compared to traditional health care settings — to health care providers, insurance companies and state agencies.
"If you treat people actively using, you save money in the long run," de Gijsel said. "That's the purpose of this trial."
The Massachusetts-based team will work its way up the Connecticut River Valley, targeting Springfield, White River Junction and St. Johnsbury in Vermont, as well as communities in New Hampshire and Franklin County in the northwest corner of Massachusetts.
"We're talking about a mobile clinic that can help you in real time to learn your status and access treatment," Daltry said of the van-based program. "That's pretty hard to beat."
Contact Dan D’Ambrosio at 660-1841 or ddambrosio@freepressmedia.com. Follow him on Twitter @DanDambrosioVT. This coverage is only possible with support from our readers.
This article originally appeared on Burlington Free Press: Health care providers target hepatitis C in rural Vermont

