Highmark said a 6-year-old's treatment wasn't covered. The community changed its mind
EDITOR'S NOTE: This story has been updated to correct that the branch of Highmark that initially denied the request for coverage was Highmark Blue Cross Blue Shield Delaware, not the provider's Medicaid provider.
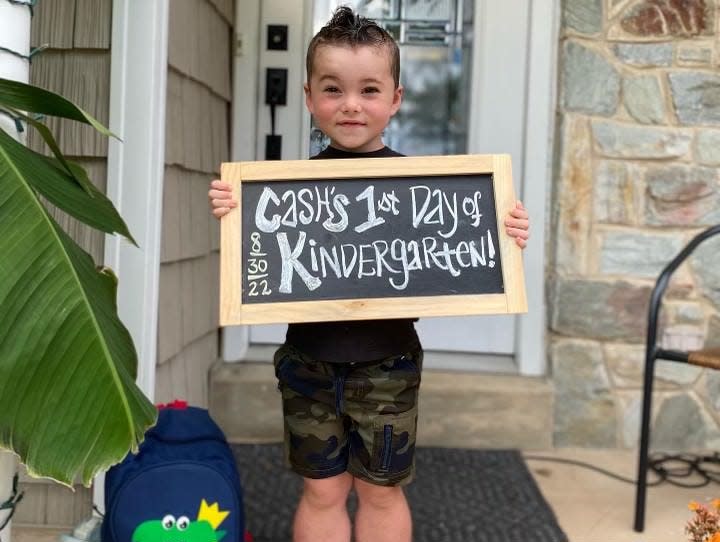
Six-year-old Grant "Cash" Huber knows he’s different.
He’s always been fascinated by the way things work, mom Jena said, and he’s very aware of his surroundings. He understands that his abilities aren’t the same as his peers; he often needs to rest more and can’t run around like his brother.
Cash has a rare genetic disorder called Duchenne muscular dystrophy. It’s caused by a lack of the protein dystrophin, which leads to the degeneration and weakness of the muscles, according to the Muscular Dystrophy Association. This form of the disorder primarily affects boys, and symptoms often occur in early childhood.
But in June, the Huber family was filled with a new hope: the Food and Drug Administration had approved a new gene therapy called Elevidys to treat Duchenne muscular dystrophy in children between the ages of 4 and 5.
INSURANCE: Nurses say they were never told Medicaid reimbursements went down. Now they want answers
Cash was still 5 at the time his parents began the application process, father Phillip explained, and he was soon approved to receive the treatment at the Children’s Hospital of Philadelphia.

The Hubers then applied for coverage from Highmark Blue Cross Blue Shield Delaware. They submitted the paperwork three times, even including an appeal from their doctor at CHOP.
Each time, Highmark denied them coverage. Phillip said the company told him that the drug was experimental and not medically necessary.
A spokesperson for Highmark Health Delaware said she could not comment on the case because of medical privacy laws.
When it became clear that appealing their case would not be enough to get Highmark to reverse their decision, the Hubers created a petition on Change.org on Aug. 20 urging people for their support in convincing Highmark to provide coverage for the Elevidys.
Four days later, the Huber family received the news that the company had changed its mind.
HEALTH: $10M is on its way to Delaware organizations tackling the opioid crisis. Is it enough?

Phillip said he called his wife while she was at work to update her on the decision, and she could immediately tell from his tone that it was good news. The two laughed and cried together over the phone, both thrilled and in disbelief that they’d managed to overcome this hurdle so quickly.
“This past week has been really emotionally draining,” Jena said. “It’s kind of been like a roller coaster ride.”
Jena said that when she left work on Wednesday evening, the petition had about 7,000 online signatures. By the time she got home 45 minutes later, it was up to 10,000.
When the petition closed on Friday, it had received over 35,000 signatures.
“It just shows how much the community can pull together when they see something is wrong and how much power they have in the strength of numbers,” Phillip said.
It wasn’t just the virtual signatures. Community members and advocates from the Little Hercules Foundation and the Parent Project Muscular Dystrophy – both organizations dedicated to fighting to end Duchenne muscular dystrophy – helped apply pressure on Highmark.
MORE: Delaware child abuse investigator positions are largely vacant, leaving workers overloaded
They called the company and sent emails, Phillip said. Some even confronted Highmark employees in person.
The insurance company’s decision to cover the gene therapy “opened the door for a lot of other children, too,” Phillip said, “which is just the most phenomenal part of the whole thing.”
Other parents of children with Duchenne muscular dystrophy have said that the treatment has helped immensely, with one mother sharing that her 9-year-old is even playing soccer.
“Our son has never jumped or ran in his life,” Phillip said. “He walks fast, but he's never left the ground. So we're looking forward to that day.”
Jena said she can’t wait for the day that Cash can run and play with his younger brother.
“It's just really exciting to think about him having the boyhood that he deserves.”
Send story tips or ideas to Hannah Edelman at hedelman@delawareonline.com. For more reporting, follow them on Twitter at @h_edelman.
This article originally appeared on Delaware News Journal: Muscular dystrophy treatment for boy approved by insurance after fight

