Hospitals complain problems persist a year after L.A. Care was hit with record fines
A health insurance plan that serves poor and vulnerable patients in Los Angeles County was slapped with record fines — $55 million in total — last March for what a California state agency described as "widespread, systemic, and unrelenting" failures, including sluggish authorizations for medical care that left patients suffering.
A year later, Southern California hospitals complain that problems have persisted and are reaching a crisis point. The Hospital Assn. of Southern California and other healthcare groups have urged the Los Angeles County Board of Supervisors to call for changes from L.A. Care, a publicly operated health plan that serves more than 2.8 million people, most of them on Medi-Cal.
What worries medical staff is "that this is putting people at risk," said Dr. Jorge Reyno, senior vice president of population health for MLK Community Healthcare.
Hospital officials have faulted L.A. Care for delays in authorizations that are needed for medical care or to discharge people to other facilities, clogging hospitals with patients who no longer need their beds. The lag time has been exacerbated, they said, by a growing number of providers unwilling to accept L.A. Care patients because the health plan has not paid them promptly.
L.A. Care has defended its performance, calling the letter from hospitals a “blatant mischaracterization of the issues.”
It said it “works tirelessly to find places to accept members” when they no longer need a hospital bed and has been taking steps to address such concerns. But it argued that the problems faced by hospitals are rooted in the broader problem of low rates of reimbursement under Medi-Cal.
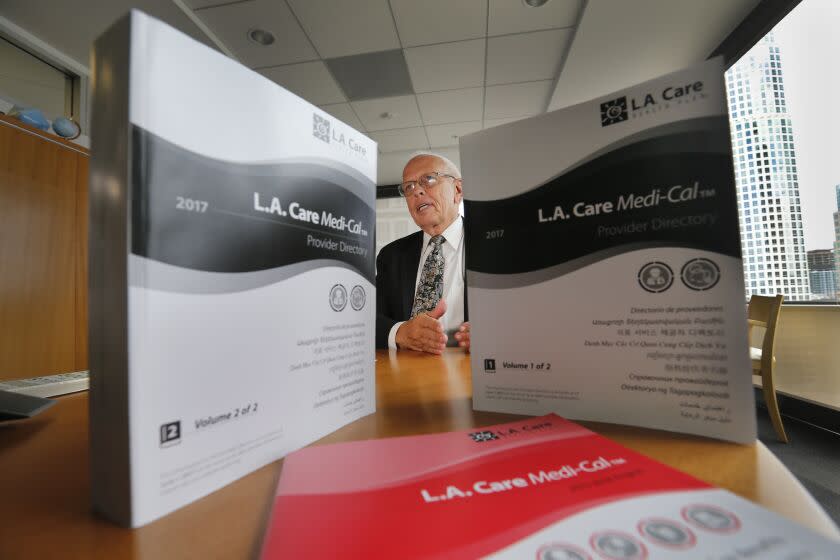
The fundamental issue is that when Medi-Cal patients need to be discharged to skilled nursing facilities, "if they can fill a bed with a Medicare patient, they can get a much better reimbursement. If they can find a private pay patient, it's even better," said John Baackes, chief executive of L.A. Care.
"We're not the problem," he said. "It's really a more systemic issue."
L.A. Care has operated a managed care plan for Medi-Cal patients in L.A. County for more than two decades. The organization, created as an independent public agency by the state of California, is overseen by a board that includes representatives from groups involved in healthcare, including hospitals, community clinics and the county Department of Health Services.
In its accusation last year, the California Department of Managed Health Care said that L.A. Care delays had harmed patients, including a cancer patient who deteriorated rapidly as he went without treatment.
Another L.A. Care member, who had been told they might have only six to nine months to live, ran into "consistent denials and delays" from L.A. Care in obtaining treatment — and abandoned the health plan as a result, the department wrote.
Baackes said that for delays in authorizations and grievances, "today I can say those problems have been addressed." L.A. Care is contesting the amount of the fines from the Department of Managed Health Care and the Department of Health Care Services and has not paid them as it pursues its appeals.
The Department of Health Care Services said it has been working with L.A. Care to address the root causes of its problems, and that L.A. Care had been keeping pace with new requests for prior authorizations after clearing a backlog.
The Department of Managed Health Care said it was also continuing to monitor whether L.A. Care is following state laws. Its last routine assessment — which covered a period from June through September 2021 — found repeated deficiencies, including that the health plan had improperly denied claims. Both agencies said they were reviewing the concerns raised by the Hospital Assn. of Southern California.
In interviews, hospital officials said they had struggled to transfer out L.A. Care patients who no longer needed a hospital bed.
One L.A. Care member who could have been discharged a day after being admitted to a Providence hospital in Tarzana instead stayed for nearly three months as the hospital was turned down by sub-acute facilities, said Dr. Bernard Klein, chief executive of Providence Holy Cross Medical Center.
"When you call L.A. Care, there is not a lot of support or help," he said. "The burden falls on the hospitals."
Klein said that another L.A. Care member who had stabbed himself in the knee was treated, and then needed to be transferred to a nursing facility, but one after another turned the hospital down. L.A. Care refused to authorize another kind of placement and said the hospital had to keep looking for a nursing facility that would accept him, Klein said.
The patient ended up spending 132 days in the hospital — 98 days of which were "avoidable" — "because we could not find a place to place him," Klein said. Providence ultimately decided to pay $15,000 to move him into a board-and-care facility for months, Klein said, in order to free up his hospital bed for other patients.
At MLK Community Hospital, patients had to spend roughly 600 additional days in the hospital last year, “just due to administrative issues related to L.A. Care,” Reyno said. The health plan accounts for roughly 55% of its admissions, but more than 70% of its "administrative avoidable days," he said.
And Dignity Health, which has several hospitals in the L.A. area, said that on average, L.A. Care members remain in the hospital for four days longer than when they would be expected to be discharged.
Its care coordination teams often reach out to L.A. Care, but "they don't get direct intervention and help in terms of how to solve these issues," said Dr. Raheem Kajani, vice president of population health clinical operations for its Southern California division.
Hospital officials said that as L.A. Care members linger in hospital beds, it becomes harder to move patients out of the emergency department and into inpatient care, and that as emergency departments fill to bursting, it takes longer for paramedics to offload new patients. That snowball effect hurts not only L.A. Care members but anyone who needs a bed or an ambulance, the hospital association and other groups argued.
"If an ambulance is sitting in the emergency room waiting for a bed, they're not available to run a 911 call," said Chad Druten, president of the Los Angeles County Ambulance Assn.
His group and the California Assn. of Health Facilities, which represents nursing facilities, joined the hospital association in asking for the county board to call on L.A. Care to take immediate steps to speed up authorizations.
Los Angeles County Supervisor Hilda Solis, who also sits on the L.A. Care board, said she was "very concerned" about the delays described by the hospital association, and had spoken directly with Baackes about the issue. So far, however, the county board has not taken any official action to call on L.A. Care to make changes.
L.A. Care told hospitals that it had moved to expand its network of facilities to discharge patients and is now contracted with the 313 out of 390 skilled nursing facilities in the county. Baackes, in an interview, said L.A. Care had offered higher payments to some nursing facilities to take hard-to-place patients.
The health plan said that more than 97% of the time, its turnaround times were within 72 hours for authorizing inpatient care for urgent cases. And L.A. Care said it would soon have a dedicated team to assist hospitals in resolving authorization and discharge issues.
Hospital association President and CEO George W. Greene called it "yet another statement with little substance or mechanism for accountability" and countered that 72 hours was still far too long. In a letter, he said that even though L.A. Care had expanded its network, facilities often “refuse to accept the plan’s members because L.A. Care does not pay them in a timely or accurate manner.”
Joe Diaz, regional director of the California Assn. of Health Facilities, said some skilled nursing facilities are owed $500,000 to $750,000 in payments, and "simply can't operate losing that kind of money."
The health plan has also been sued in recent years by other companies that alleged L.A. Care shorted them what they were owed, most recently a COVID-19 testing laboratory; L.A. Care said it had not paid out anything to plaintiffs in two cases that were dismissed in recent years and declined to comment on an ongoing case. Several hospitals also said L.A. Care owed them money. At four hospitals in the L.A. area run by Providence, roughly $11 million was owed by L.A. Care more than 30 days after the claims were submitted, Klein said earlier this month.
L.A. Care said it was not delinquent in payments to hospitals or skilled nursing facilities based on "clean claims" that included all necessary information, although incomplete claims could be denied because of missing information.
The health plan also said it had increased the rate at which nursing facilities get claims accepted and paid, with more than 90% of clean claims processed within the required time on the first try.
And it argued that discharges were a statewide issue for Medi-Cal recipients because nursing facilities are not required to take all patients regardless of insurance coverage, and L.A. Care treats "a more vulnerable population of higher acuity members who are harder for [them] to treat and eventually discharge."
When California regulators announced the record fines facing L.A. Care, they accused the health plan of failing to maintain enough employees to properly process authorization requests, even though "its financial assets were vast."
L.A. Care said the past backlog was not simply the result of staffing issues, but that it had overhauled the department that handles those authorizations, increased its staffing, and has now been operating seven days a week to support discharges to nursing facilities. It argued that its financial reserves were on the low end compared with its peers.
Hospital officials around Los Angeles County said their issues with L.A. Care are not new, but have become more dire as medical facilities across California are under stress. As the San Joaquin Valley reels from the recent closure of Madera Community Hospital, the California Hospital Assn. has warned that more hospitals could be on the brink of closure. It is seeking a state infusion of $1.5 billion to stabilize them, arguing that federal aid failed to cover the financial losses that California hospitals incurred during the pandemic.
More patients are back at hospitals, "but the patients who are in there tend to be sicker than they were pre-COVID," said Glenn Melnick, a USC professor focused on health finance, and "the prices they have to pay for people to take care of those patients is up," due to surging prices for labor and supplies.
"The COVID clouds have cleared, but new clouds have now taken their place," he said.
The California Hospital Assn., like L.A. Care, has argued that Medi-Cal is underfunded. But it has also urged the state to step in and demand that health plans immediately pay outstanding claims, saying that "immediate action is needed to hold health plans accountable for meeting existing requirements in state law."
This story originally appeared in Los Angeles Times.

