A Hustler’s Guide to IVF

Since 1972, approximately 8 million babies have been born using Assisted Reproductive Technology (ART), a set of fertility treatments in which eggs, sperm, and embryos are handled outside of the body. According to a 2018 Pew Research report, about a third of American adults have either done some form of ART or know someone who has. The most common kind of ART is In Vitro Fertilization (IVF).
IVF is a gamble. It’s betting the farm on a slow horse with crap odds, hoping for a miracle payout. A true hustler is an obsessive gambler with an insatiable need to pursue that payout at all costs. In this case, the payout happens to be a baby.
Damon Runyon, the famous writer of Guys and Dolls, and a man who crafted the perfect picture of low-level hustlers, once said, “you can become a winner only if you walk over the edge.” Over the edge I have been, on a manic quest to meet my kid.
Going through the IVF process, I felt more like the characters outside of an Off Track Betting, or a hungry gambler at a craps table, than I felt like a person trying to get pregnant. Where they may have been clutching racing forms and chain-smoking cigs, I was scribbling notes about embryo gestation and gobbling vitamins. All of us relentlessly betting in a game which often ends in the memory of the race and none of the spoils.
At 36, I had already been divorced, and decided I wanted to travel the world and train in combat sports. I had been left by my first husband for another woman, but before I knew that, the excuse given was that he didn’t want to “waste any more of my time” if I wanted kids, and he was no longer sure that he did. My fertility was used as a way to frame leaving as a favor, and to avoid the unpleasant admission that he had simply fallen in love with someone else. This was the first time I thought about the fact that my ability to bear children was finite.
After we separated, I wasn’t feeling hopeful about lifelong partnerships in general, and the idea of getting right back on the horse, with “the clock ticking,” hoping to find a man, fall in love, and have a baby, seemed absolutely absurd. It all sounded like a hell of a lot less fun than learning Muay Thai in Bangkok, and writing from Southeast Asia for a few years. Of course, as fate would have it, I met Adam a week before leaving for Thailand, and we corresponded the entire time I was there. I came home, and the rest was history. The timing and chemistry had seemed like a romantic comedy and unrealistic. We both knew early on and with very little discussion that we wanted to be together and start a family, which was the last effortless thing about trying to have a baby.
When we started, I knew almost nothing about the way my body functioned in regard to fertility. I just had a vague sense that some women had to go to a doctor to get pregnant. After a few months of sex at the right time without resulting in a pregnancy, I got antsy and wanted answers. Those answers, as it turns out, were hard to come by, in part because I knew so little about reproduction and the way my body worked. I barely knew what I wanted to ask.
What I did know about my body—period, ovulation, sperm meets egg, baby grows in uterus—was woefully insufficient. It wasn’t even a true picture of the basics. It felt like I was starting to play a high-stakes game and needed to learn the rules along the way. There are very few resources for the layperson that cover, toe to tip, the process. From the phases of a reproductive cycle to how embryos gestate, the more I found, the more I learned, the more I found I didn’t know.

Choosing to Play the Game
There are a lot of different reasons to use medical intervention in conception: maybe you ran out of eggs, or the eggs you have aren’t “viable,” maybe your cycle isn’t regular, or your womb has an issue, or the sperm isn’t fast, or you’re in a same-sex partnership and want some of your own DNA involved, or you’re starting a family as a single adult, or you share the recessive gene of a genetic disease with your partner, and so on, and so on. In my opinion, no reason is better, worse, or worth more than any other. The reason is only truly relevant when navigating the slippery and slimy world of paying for it, but we will get to that later. My personal reason was that I was in my late thirties with the vague diagnosis of “unexplained infertility,” and I didn’t want to wait or have a miscarriage if I could avoid it.
Between the ages of 36 and 40 the rate of miscarriage increases from 15 percent to 29 percent. I have several friends who went through at least one if not two losses trying to conceive in their late thirties. Some miscarried at two months, some at four; I didn’t want to take that emotional hit if I didn’t have to. Asking myself how many miscarriages I was willing to risk or endure, as opposed to the rigorous process of fertility intervention, was all part of the kind of grim calculations that I would need to grow comfortable with.
Still, recently, I did have a miscarriage, and it confirmed for me that it is something I personally should go to great lengths to avoid. Testing the tissue afterward revealed that it had been caused by a chromosomal abnormality in the embryo. Most miscarriages, especially in older people, are caused by chromosomal abnormalities, also known as ‘aneuploidy.’ According to a 2021 report from the National Library of Medicine, chromosomal abnormalities affect “10-25 percent of eggs in women in their early 30s, and more than 50 percent of eggs from women over 40,” making it “a leading cause of miscarriages and infertility.”
To combat this, embryos can be tested before being inserted back into the uterus—a process called Preimplantation Genetic Testing, or PGT. Once testing is done, only “viable” embryos are transferred back into the body. IVF is not a guarantee against miscarriage, but embryo testing reduces the risk of miscarriage significantly, and embryos can only be tested if they are on the outside of the body.
For many people, the possibility of a miscarriage, two, or three is worth a natural conception.
Whether it’s for spiritual reasons or due to prohibitive costs, the calculus is different for everyone. I would trade two miscarriages for a belly shot full of hormones and quick surgery any day of the week, but that’s me, and I’m not saying IVF is a walk in the park either.
I had trouble reconciling my desire to have a baby with the indifferent and effortless persona which I wanted to portray. Even though Adam and I were actively trying to conceive, I never wanted to betray my earnest yearning for a baby because, in my mind, if it didn’t work out, I would be seen as pitiable and desperate. “Sure I want kids,” I would say, “but I’m never going to be one of those women who have to…” and then fill in the blank with whatever scenario I fearfully judged: track my ovulation, take a bunch of supplements, or do any kind of “sci-fi pregnancy thing,” which is how I referred to IVF at the time. With each passing month, the goal post moved a little further, and pretty soon, I was one of those women who was willing to do whatever it took, by hook or by crook.
I thought of my grandfather who, at 7 pm every night, would roll out a small felt with a craps board printed on it. He had a translucent green visor and a tiny little notebook with a tiny little pencil. He would roll and roll and take notes. He did this for years until his faculties would no longer allow it. He was perfecting his system. I started gathering my data, seeing if with enough information I could perfect a system and roll, bluff, and bet my way into pregnancy.
Finding a deficit of encouraging depictions of successful IVF in popular culture (it all often is used as a plot device to portray bleakness and struggle, hopelessness, and loss) I sought the underdogs and two-bit losers in the movies I grew up loving. The scamps that get-over in the end. Steve McQueen as Papillon who finally escapes French prison on some coconuts, Paul Newman in The Sting as a down-and-out hustler looking for revenge on an old gangster who killed his friend, and Al Pacino in Dog Day Afternoon as a bank robber trying to get some money for his trans partner for gender affirmation surgery. These characters among others let me lean into all of it, the desperation, the thirst, the chase, to bear my teeth and hurl myself into the fray. I could wear my want with a bit of swagger, and that little piece of bluster and confidence was what I needed to get me through the next few months.
Do Yourself a Favor and Stop Being Precious About Conception
Producing biological children out of my own body isn’t exactly a necessity, it's more akin to a deep, all-encompassing passion. When that passion hit me, it felt like the biggest pull in the universe. Chasing pregnancy felt both thrilling and excruciating. When I wasn’t getting pregnant, every single month created a cycle of anticipation, elation, obsession, and let down—a recipe for addiction if ever there was one.
The fear that a medically-assisted pregnancy isn’t as good or genuine as any other is one that mostly plagues heterosexual and gender normative folks. Gay, lesbian, and trans people who have the itch to start families know that medical assistance, in some form or another, is just the cost of doing business. For me, it seemed as though everyone else was just blithely falling into pregnancy with ease. I imagined I would conceive, making love in some idyllic setting like in a secluded flower field or a hotel room. Instead I was staring at fluorescent lights in a cold doctor’s office, feeling my goosebumped skin scratch against a paper gown. Sharing the experience with people for whom IVF is not the last resort, but an expected pre-pregnancy process was an incredible shift in perspective. It allowed me to be excited about it all.
I had been dogged by brain goblins that looked and sounded just like me, whispering that my age and infertility made me worthless as a woman and as a wife. I felt guilty that Adam had fallen in love with me. I thought I had robbed him of the joy of children and that I alone would not be enough. The fever broke at some point and I realized that these punishing thoughts would not make a baby. I didn’t know a lot of people that discussed fertility candidly; many people are afraid to mention it or ashamed, which creates these siloed couples feeling quite alone and unprepared as Adam and I did.
Waiting is for Suckers
Fertility works on a maddening, cyclical progression through time, where the years orbit around the monthly menstrual cycle, itself revolving around daily fluctuations in hormone levels. First is the gradual decrease in one’s ovarian reserve: people with ovaries are born with all of the eggs they are ever going to have, and mature eggs are released each month one or two at a time; however, hundreds of eggs which never mature extinguish each month. On top of that, the ovaries naturally tend to lead with ‘healthier’ eggs earlier in life. When I understood that the “ticking clock” is an appropriate euphemism, I wanted answers as fast as I could have them, but I discovered that there are a lot of gatekeeping measures to bottleneck access to fertility support.
In general, the recommendation from ACOG (American College of Obstetricians and Gynecologists) is that, if you are under 35, they want you to try “naturally” for a year before doing any kind of testing whatsoever; if you are over 35, the recommendation reduces to 6 months. Even 6 months seemed too long to wait for even initial testing. If I had a blocked tube or no eggs at all, I wanted to know upfront.
If a doctor had told me to wait, I would have gone to a different doctor and said what I had to say. To me, these are arbitrary requirements that only benefit insurance companies to the detriment of reproductive health. Luckily, we do not yet live in a world in which, by law, our bodily functions and sexual activity are tracked and the data automatically shared with our medical providers. My doctor had to trust that the amount of time I claimed to have been trying was accurate.
My first gauntlet of tests would provide my diagnosis.
HSG or Hysterosalpingogram is an X-ray of your fallopian tubes and uterus. This is to spot any blockages in the tubes or defects in the uterus: a useful thing to know because some blockages are treatable and in some cases doctors advise patients to move straight to IVF.
FSH blood tests measure the “Follicle-Stimulating Hormone,” which prompts the ovaries to make mature eggs each month.
AMH Level blood tests measure the “Anti-Müllerian Hormone,” which, among other things, can predict how plentiful one’s ovarian reserve is. An ovarian reserve indicates how capable the ovary is to provide “egg cells.” If the ovarian reserve is too low to reasonably expect fertilization, many people pursue alternative options such as egg donation.
Male fertility assessment. It’s a no-brainer to test the ejaculation for sperm count and sperm mobility before I underwent a bunch of pokes, prods, X-Rays, and ultrasounds.

Know Your Handicap
My fertility doctor said something very useful to me at the start: “Eggs get old, uteruses don’t.” It’s good to know what you have going for you. In our initial consultation, she asked me if I had ever been pregnant. I told her that I had, as a teenager, and that it had ended in termination. It was the first time that fact about my history was an encouraging reveal.
“Oh,” she said, raising her eyebrows.
“Is that bad?” I asked, worried that I had harmed my uterus with an abortion.
“Not at all,” she answered. “It’s good information. We know that you can get pregnant.” She explained that abortions do not harm the uterus or make it harder to get pregnant, if they are done properly by medical professionals.
I also looked at my family history. Most women on my mother’s side had stopped having kids by their early thirties, and there were a few stories of miscarriages beyond that age.
The results of my initial tests came in. My ovarian reserve was high, above average, according to her. There were no polyps or blockages, the pipes were all clear. My diagnosis was “unexplained infertility”, which is common for people in my age group.
Even if my blood was saying that I had a big ovarian reserve, there was no way to tell how many of my eggs would go on to become feasible embryos until we scooped ’em out and took a look at how they developed. My uterus looked fine in the ultrasounds, but what did we really know until we put an embryo in to see if it would take. They can gauge a lot but the rub is that sometimes in order to truly diagnose the issue, doctors just have to try it out and see. It’s a hell of a hard way to find out what you have going for you.
My doctor suggested IVF as it was the quickest way to get pregnant with a reduction in the possibility of miscarriage—but me being suspicious of the waiter that always suggests the lobster, I wanted to know what the other options were. We were told about medication that can stimulate ovulation, or something called IUI (Intrauterine insemination). Medication is administered to control ovulation, the cervix is dilated, and sperm is inserted directly into the uterus. The success rates of these options were almost as low as just trying naturally. If my diagnosis was different—if my infertility had been due to an irregular period or endometriosis, and I was a few years younger—maybe I would have rolled the dice on these methods. I decided to go straight for IVF. I ordered the lobster. I wanted the quickest, best shot at getting pregnant.
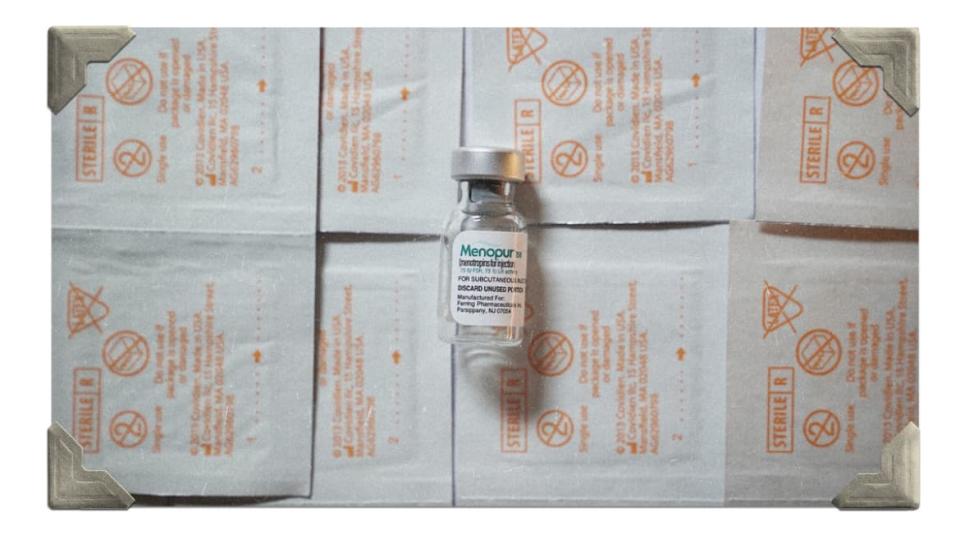
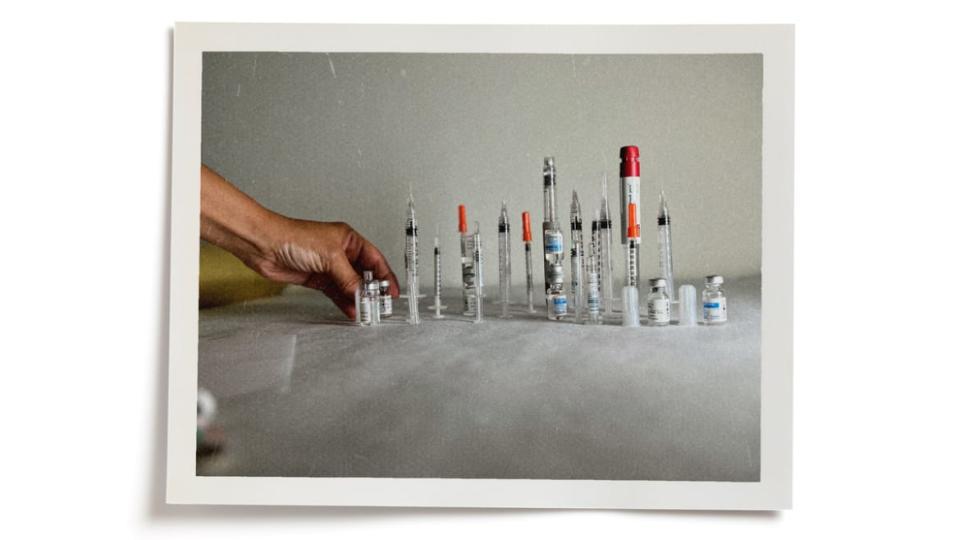
We picked up our medication, which was about 16 days’ worth of various hormones in tiny bottles. Some needed refrigeration and some didn’t. We got alcohol wipes, syringes, and a little bio-waste bucket for the used needles. We quarantined ourselves, because we did not want to get COVID during this process: if I did, the doctors told me, they would halt the cycle—no ifs, ands, or buts—wasting the insurance money, the medication, and the time.

The Nitty Gritty
Everything was going to start with the first day of my period. The hormones, the monitoring, everything. Waiting to see blood, aware of every twinge and cramp, I felt like the horse in a racing movie, chomping at my bit and hoofing the dirt in slow motion, breathing out, wide-eyed, waiting for the bell to ring and the gates to fly open.
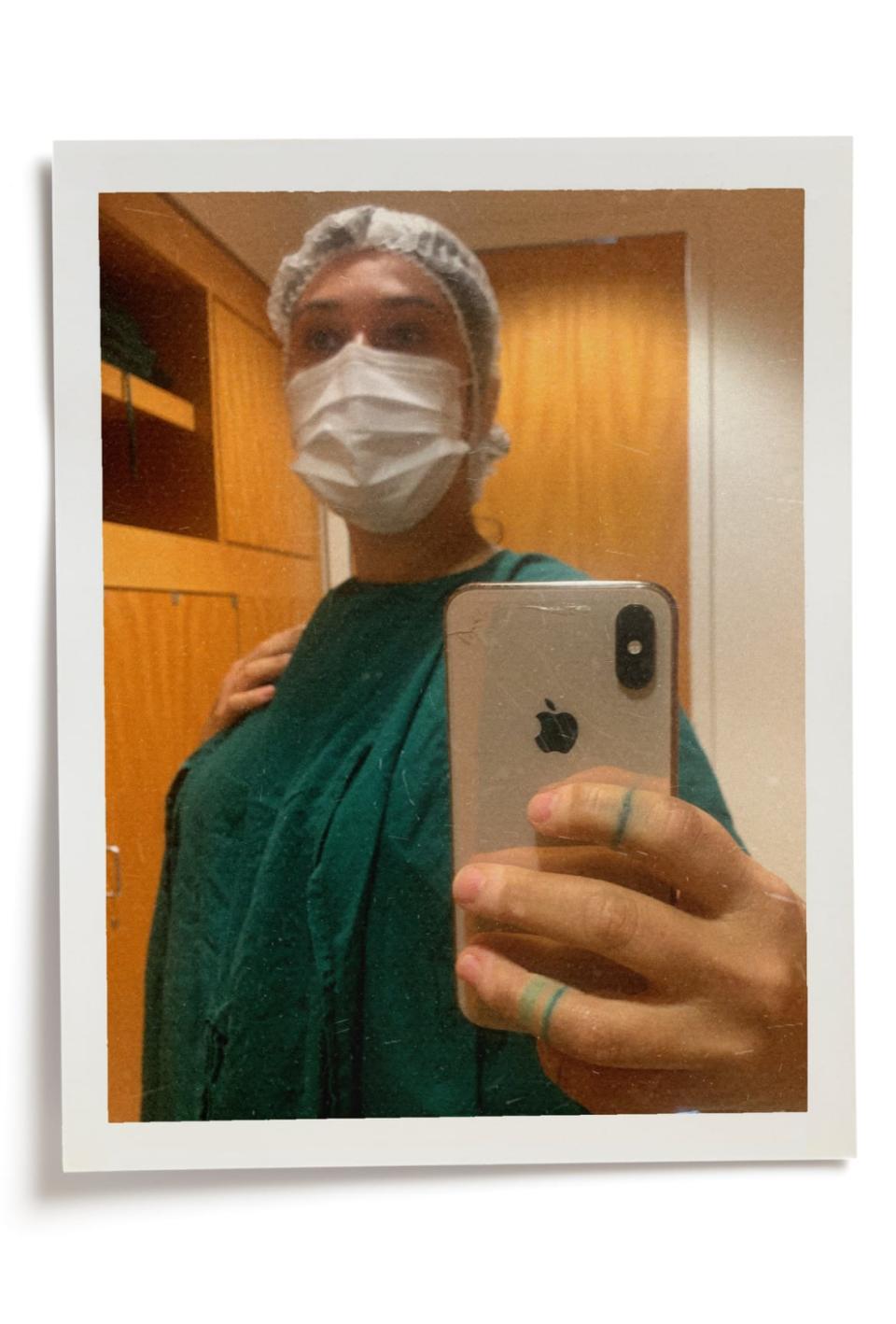
On day two, I went in for my tests, and would go in every two days thereafter. They monitored my hormone levels so they knew when to adjust the medication and anticipate ovulation. After two weeks of this, the veins in my arms were pretty bruised up. Twice a day, my husband and I mixed and shot the medication into the fatty tissue on my abdomen. Every three of four days I got an ultrasound to see how big the follicles in my ovaries were getting, which would indicate how many mature eggs would develop.
The medication causes the ovaries to produce more mature eggs than usual. How many more is really a crap shoot and depends on a slew of factors like age, genetics, and a few unknown variables that science cannot explain yet. The same person can have two egg retrieval cycles, seemingly exactly the same and one cycle could produce 20 eggs and the next could produce five.
The shots didn’t hurt, and if I’m honest, I liked the druggy ritual of it all: it made me feel like I was tough, like I had it all in control as long as I followed the steps, mixed right, and kept my surfaces sterile and my needles in a row. It was also a nice way for Adam to physically participate, and having him there with me made me feel close to him. Occasionally a curious friend would watch the process and we would giggle at the self-serious instructional videos. I gained 13 pounds in a month, and wasn't allowed to exercise (doing so could cause an ovarian torsion, which has terrible consequences). I didn’t love that.
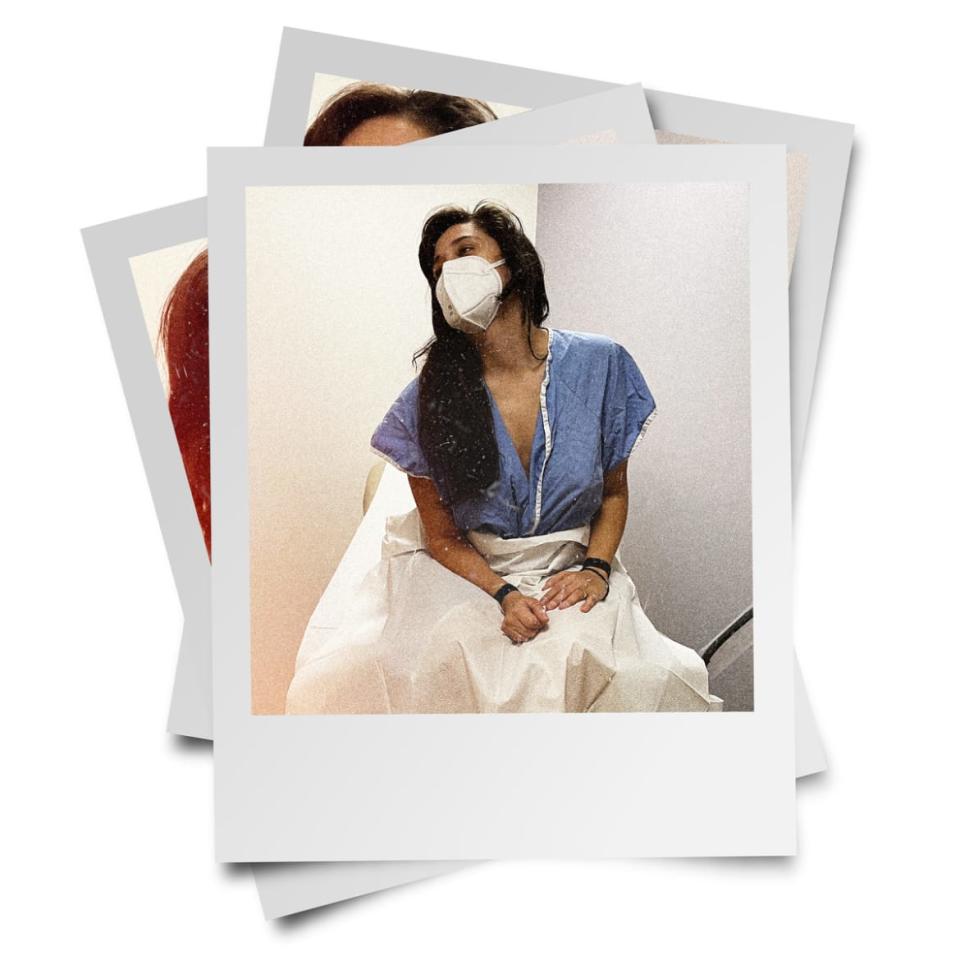
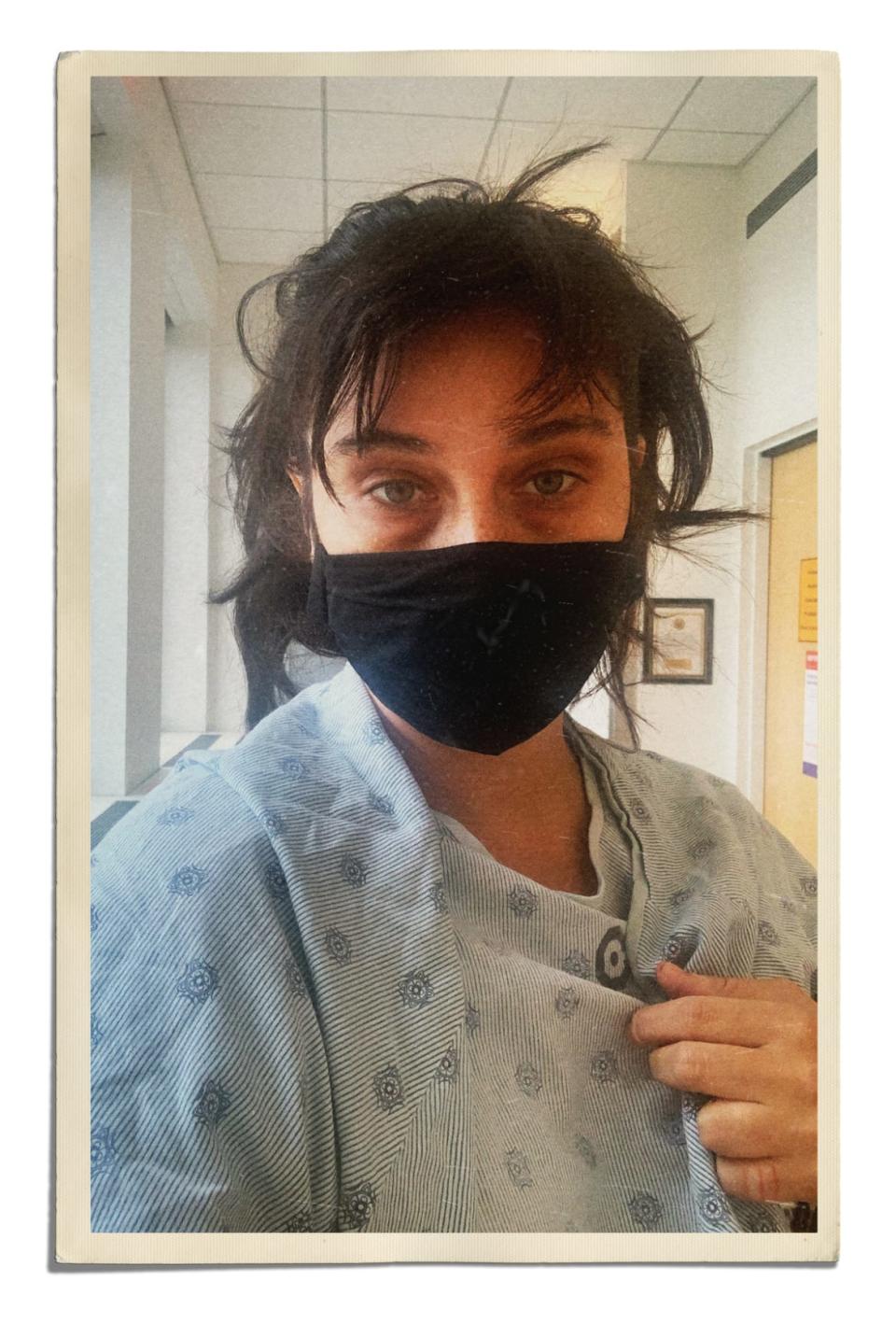
After a fortnight, it was time to ovulate, so I took the “trigger shot,” and 48 hours later I was at the clinic to do the egg retrieval, which I like to refer to as “the harvest.” I sat in a row of cozy lazy-boy chairs with other patients all done up in medicinal blue gowns and hair nets. We all watched as patients walked out of one door and came back through another. They were wheeled in on gurneys, passed out in a deep drug sleep. My procedure took about 15 minutes. When I woke up they were able to tell me how many eggs they got, and by the end of the day they called me with how many had fertilized when mixed with Adam’s sperm.

The Pressure is On
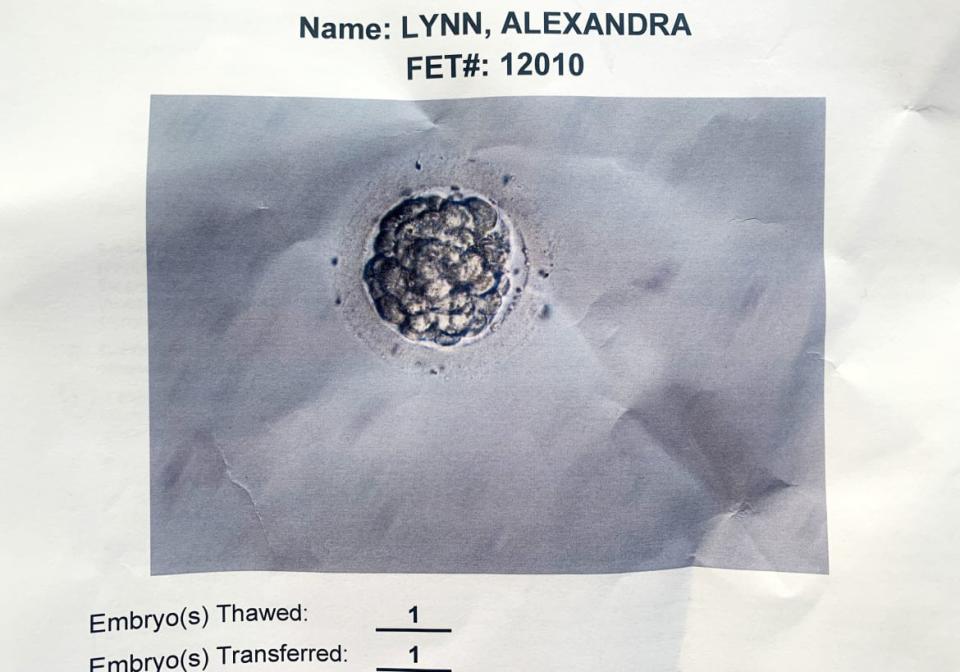
Out of 15 eggs retrieved, 9 of them fertilized; 5 days later, only 4 had made it to blastocyst, the name for a pre-embryo embryo.
Our clinic froze our four blastocysts and sent a sample off for testing. The lab would take 5-7 days to get us results. I was told to expect a heavy period approximately 10 days after the egg retrieval. Ideally, I would know how many blastocysts were viable—meaning, how many would not miscarry due to chromosomal or structural abnormality—before starting the next cycle which starts with the period. It would determine whether we tried for a second retrieval or a transfer cycle (where they put the burgeoning embryo back in to see if it grabs on.) Retrieval cycles are more expensive than transfer cycles, so you don’t want to waste the money or the insurance allotment if you don’t have to, but it is really down to the wire between when you get your results back and when your period starts.
Beware the Madness
We finally got the news that we had only two viable embryos out of the original four. I was surprised. It was a very stark reckoning with the odds. This sent me into a strange mental spiral akin to what Dostoyevsky referred to as “brain fever,” for his characters wracked with love or debt or religious fervor; I felt like I was mired in all three. I became determined, my vision tunneled and my chances of success were all I thought about. “But gamblers know how a man can sit for almost twenty-four hours at cards, without looking to right, or to left,” writes Dostoyevsky in The Gambler. Once I was in it, I was all in. I didn’t want to stop to grieve or take a break. I worried that if I stopped, I may not have the mental strength to start again.
Trying to control the odds of any situation is, essentially, the hustle. It was in that spirit that I went about a rampant pursuit of any kind of guarantee. I collected statistics from the Center for Disease Control (CDC) and the European IVF Monitoring Program (EIM) about people in my age group, with my ethnic background, in my country, even the success rate of my clinic. I would stay up at night using dice simulators to see if I could predict my chances. It was a roundabout way of just shaking a Magic 8 ball over and over again. I couldn’t stop thinking about it. It was like there was a rat in a maze functioning as my brain, and no matter which corridor the rat scurried into, it did not lead me to anything resembling control. I thought about it all day, every day until I went in for my next egg retrieval.
11 mature eggs
8 fertilized
5 blastocyst
0 viable embryos after testing.
My doctor provided me a list of every single chromosomal abnormality on each one of my tested embryos; some had more than one. None were even “mosaic,” which would mean that there were both abnormal and normal cells detected and they could test again. After a few hours of research it seemed as though it was highly unlikely that any of these embryos, even if they did implant, would make it past a few months of pregnancy.
I found studies done in which the researchers said that there was a slight possibility that some chromosomally abnormal embryos can self-correct. In desperation, I glanced through a few websites run by religious zealots. I wanted the hope they were selling so badly. My doctor talked me through the studies and explained that the science was so far away from being meaningful to someone pursuing a healthy pregnancy.
After all this I needed a break from the hormones, so we decided to go for a transfer.
The Transfer
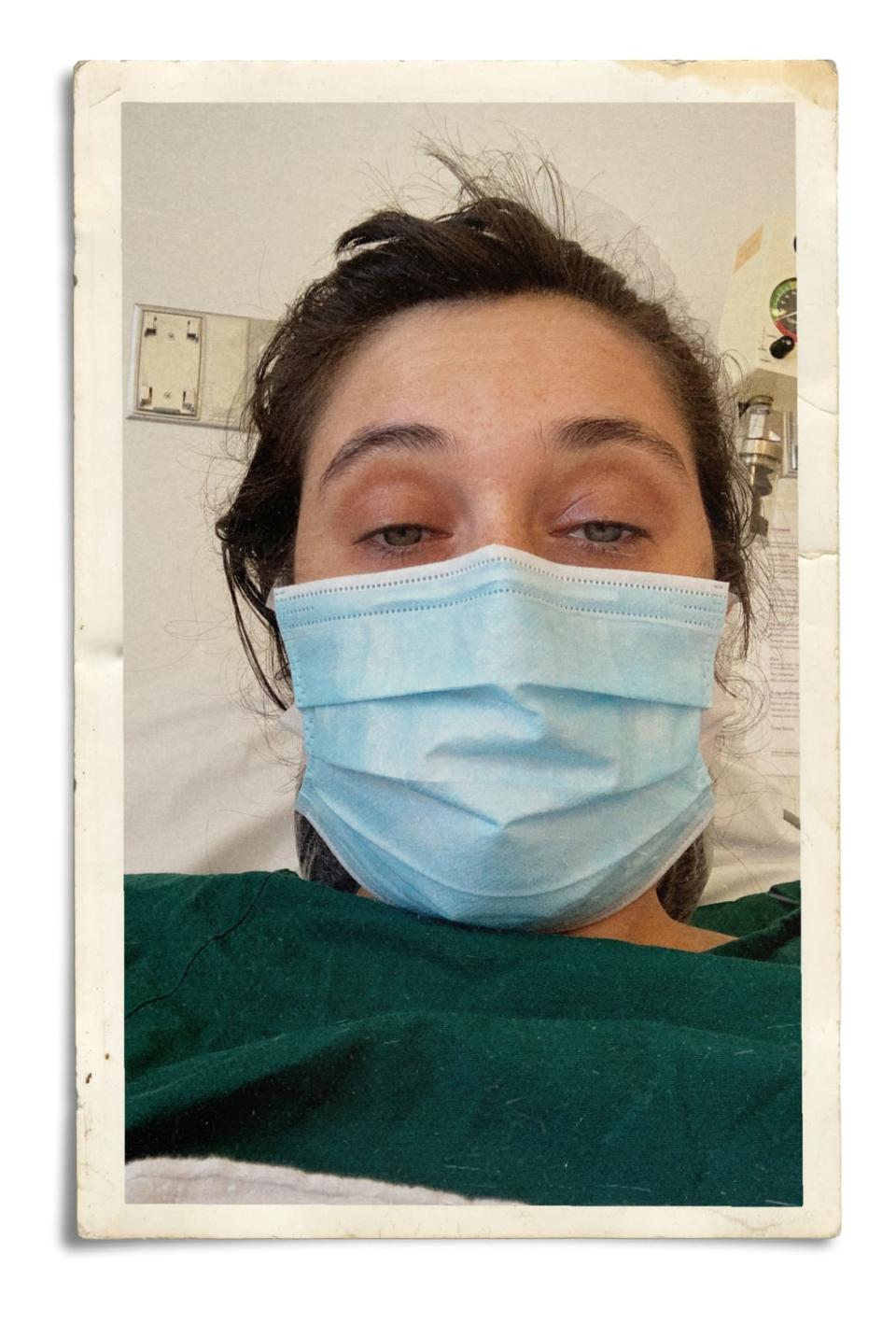
This procedure is much less stressful than an egg retrieval. You go into the clinic, they give you some valium, they thaw the embryo, thread a tube through your cervix and send it up there. I was awake for this procedure. Sometimes embryos get destroyed on thaw, which is another bleak possibility one has to be aware of and prepare themselves for, and hopefully there are enough embryos for a back-up.
After the transfer Adam was waiting for me outside in our 1987 Cadillac DeVille beater with a plush deep red interior. It struck me how much it seemed womb-like in there, with the warm lighting of the interior wall sconces. It was November 3rd, 2020: Election Day. He hadn’t been able to hold my hand during the transfer because of COVID restrictions. I curled up in the car next to him as he drove me to my post-transfer acupuncture session. It was the coziest I had ever been.
The Two-Week Wait
After the procedure we waited nine days before going in to have my hCG hormone tested. Its actual name is “Human chorionic gonadotropin.” It can be detected in the blood after an embryo implants into the wall of the uterus.
You get a blood test in the morning and wait for the results in the afternoon. When I answered the phone I immediately asked if I was pregnant.
“Well,” the nurse said, “yes and no.”
Adam, who was sitting next to me, just threw his hands up and laughed. “Of course,” he said, “why would any stage of this be easy?”
The nurse informed us that my hCG level was very low, which “usually” meant a “biochemical” pregnancy, or, as I understood it, a pregnancy that would not last, and most likely would be washed away with the shedding of my uterine lining during menstruation. My hCG level was at about 11 IU/L and, I was told, they “like to see levels between 60 IU/L and 100 IU/L.” As we have established, I’ll never abandon a long shot, so trying to find any angle to hold on to, I asked, “what precisely do you mean by ‘usually’?”
Turns out there was a slim chance that the embryo could have implanted “late.” Mostly embryos will start sticking to the uterine wall within 24 hours after transfer, but occasionally they take a day longer. The hCG hormone doubles every 48 hours at the start of a healthy pregnancy, which meant that if my embryo implanted a day late the number 11 was still low, but I’d take it.
I wanted to know exactly how often an embryo implanted “late.” The nurse sighed, “I don’t have those numbers,” she said. By now, they were used to my questioning after I got a piece of information I wanted to change. “I’ll have to have the doctor call you back.” Later, my doctor explained that it was impossible to have proper data on late implantation because most pregnancies are not monitored to the degree that IVF pregnancies are.
“Anecdotally,” I said, grasping at straws, “how often would you say you see numbers this low turn into a healthy pregnancy?” At this point I think my doctor knew what I needed. I needed the odds. I needed to give a numerical value to my Goliath. “Fifteen percent of the time,” she said, “Maybe twenty.”
I immediately felt better. I went to my bathroom doorway and kissed the mezuzah that I got after a friend asked his Rabbi where to place them for fertility. I lit the ritual fertility candles that another friend at the pagan supply store had made for me. I touched the picture of our embryo taped to the wall above a bowl of rose petals on my nightstand, and closed my eyes. “Fifteen percent ain’t nothin,” I thought.
The Stakes
Fertility is big business in the U.S. It’s lucky for all and very rare that in this case, the interest of capital and the interest of the greatest good align as Americans grapple over control of reproduction and family planning. Medically assisted reproduction is a way bigger money maker than abortions and various brands of religious zelotry may sqwak about lab created embryos. The Pope for instance said that “Making children rather than accepting them as a gift,” was “a sin against the creator,” which makes sense for someone who is interested in maintaining a monopoly on immaculate conception. All the heavy hitters: “big pharma,” and “big hospital,” and even the “big medical equipment industry,” have an interest in keeping IVF as legal as can be.
Clinics and individuals want the same thing: a healthy baby born, after an uncomplicated pregnancy, in the least amount of IVF cycles possible. For the clinic, this gets their numbers up, which will garner them more customers, more research subjects and possibly more fiscal allotment from their parent organizations. Prospective parents want to save money and bring home their child as soon as possible.
How much money it takes to get IVF will depend on where you live, who your partner is, and how willing you are to find the angles. In countries like France and the UK, up to three rounds of IVF are entirely free under their socialized healthcare systems.
The very approximate numbers in the U.S. are as follows: $15,000 for an egg retrieval cycle, with $5,000 on top of that for medication. A transfer cycle is less, it costs between $2,000 and $4,000 depending on medication. Freezing the embryos is an initial cost of $1,500 and $1,000 per year to store them. Our clinic charged us $300 per embryo to extract a sample, and the lab charged us about $400 per embryo to do the test—bringing the total per embryo to $700 for testing.
The first thing I did was find out what my insurance coverage was and what the laws in the state were. Just because state insurance must cover IVF doesn’t mean that everyone in that state will be covered, for instance if a person has federal insurance.
Adam and I are lucky. We lived in New York, are a cis-gendered heteronormative couple, and Adam works at a company which has a lot of employee benefits for fertility, including unlimited medication coverage. Most Americans are at the mercy of what insurance companies and the state define as “medically necessity.” A diagnosis of infertility constitutes a “necessity.” Infertility is defined differently in every state. Some states have discriminatory language defining infertility narrowly, in the context of sex between a man and a woman, which gives insurers a loophole with which to withhold coverage. In Illinois, however, the definition was expanded to persons with an “inability to reproduce either as a single individual or with a partner without medical intervention.” This opens the door for single parents and same-sex couples.
A person can change insurance companies and pay a premium for a year which will eventually cost less than IVF out-of-pocket. Cigna is currently the front-runner in fertility but it’s only available in 13 states on the healthcare exchange unless offered by an employer.
There are some folks, especially same-sex couples, who may take on a second job going to work for a company specifically for their inclusive fertility insurance coverage. A woman recently became TikTok famous for blogging about her part-time job at Starbucks where she takes home zero dollars for work, but is fully insured for the monetary equivalent of three rounds of IVF.
Then there are grants. State grants often only work with select hospitals. Special interest grants cover anyone from people who make less than $40K per year to people who have cancer. There are grants for certain genetic disorders, or religious affiliation. A few wealthy folks have started grants after they, or their family members, struggled with having a child—some examples being Samantha Busch, and Pamela Hirsch.
Some clinics participate in a program called Bundl which offers to package IVF cycles and sells insurance for a few extra thousand for a some-money-back guarantee if you don’t become pregnant. Most other financing plans which I won’t promote are just as predatory as one would expect.
And finally there is an entire IVF tourism industry where one can travel abroad to find cheaper ART in places like Spain, Greece, and Czechoslovakia.
Is It Worth It?
I don’t know how I would feel if it hadn’t worked, but I do know I would have always regretted not trying at all. My son is now one year old, and his name is Walter Cadillac, named after the grandfather that played craps, and the car that drove us to and from the clinic. I have no words to describe him properly or how much he means to me. It will have to suffice to say that to me, he is evidence of a kind and beautiful universe, the likes of which I had never before known. We got really lucky to get in and out of the process in 4 months… the first time.
Our second embryo which had been waiting for us, frozen in a facility in New York, didn’t take, and we are currently trying again. Hustlers like me believe in the hot hand fallacy like others believe in God, so after Walter Cadillac I didn’t think I could lose. When I did I went right back to that feeling, that passion to try anything and everything. I honestly don’t know how far it goes. It can feel like a casino at times– no windows, no clocks. If it does work, and I do hit big again, then pregnancy anxiety starts, and a new set of odds gets calculated, and it really does feel like it’s designed for those of us who will walk over the edge.
Get the Daily Beast's biggest scoops and scandals delivered right to your inbox. Sign up now.
Stay informed and gain unlimited access to the Daily Beast's unmatched reporting. Subscribe now.

