Inside the Race to Solve America's Concussion Crisis
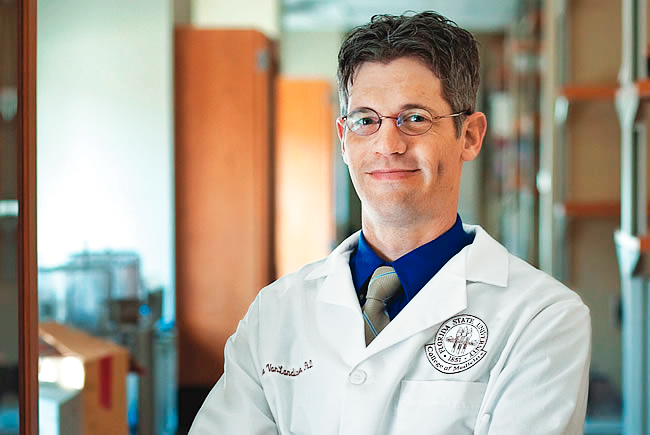
Jake VanLandingham, Ph.D., a 45-year-old neuroscientist who has spent nearly a decade trying to develop a drug that he believes can heal concussions, works out of his car. Or he sits at the kitchen table of the house he rents in a subdivision in Tallahassee, Florida. “We’re virtual,” he likes to say of his eight-employee company, Prevacus. In 2018, he says, he sold his family home to keep his start-up alive. He’d already raised and spent millions on the toxicology tests, patent applications, attorney fees, and company overhead required to take his drug into Phase 1 human clinical trials, a vital stage on the arduous journey toward FDA approval.
When I visited him in July, he steered us around Tallahassee’s live-oak-lined roads in his Hyundai SUV and explained his drug between phone calls from potential investors. When he spoke, the words emerged in an almost theatrical drawl. Born and raised in the Florida Panhandle, the scion of a clan of vegetable growers with more than a thousand acres under cultivation, VanLandingham is lean and tall, with close-cropped salt-and-pepper hair. He was dressed in a polo shirt, jeans, and a pair of flip-flops, the uniform of the Florida dad. (He is the father of four.)
VanLandingham was in good spirits. The last chunk of a promised grant would be coming through at any moment, he said. With that money, he could at last launch Phase 1 safety trials, at a research clinic in Adelaide, Australia. (Many small U. S. biotechs go to Australia for Phase 1 because it’s cheaper there.) If that were to happen, his would be the first new drug specifically targeting concussions ever to be tested in humans.
Raising funds has been difficult, he said, partly because of the confounding nature of concussion itself. Every person experiences concussion differently. Between 10 and 15 percent of people who suffer just a single concussion will go on to have cognitive problems for more than a year. No one knows why. Called post-concussion syndrome, or PCS, it can involve trouble with concentration, attention, memory, and judgment. Headache, dizziness, lack of balance, blurry vision. Sleep abnormalities, anxiety, panic attacks, depression. Children are more vulnerable to concussions than adults, and it takes longer for them to recover. As many as 1.9 million children suffer sports-related concussions in the U. S. each year, according to the American Academy of Pediatrics—up to 285,000 of them could have symptoms that last longer than 12 months. About 2.8 million people overall are diagnosed with a concussion annually, a few of them famously—in the NFL, the NHL, or even MLS—most anonymously. A fraction of those will experience concussion symptoms for the rest of their lives. Out there is the grandfather who, after a fall, has permanent vertigo. Out there is the otherwise healthy 30-year-old whose life, from the moment of a single concussion, is now punctuated by debilitating migraines. Out there is the teenager who, after a head injury, can’t get the words to unscramble on the page.
Yet the only accepted medical treatment for concussions today remains rest and time—the same as it’s always been, and the same thing you might do for a hangover. Now there’s a boom in brain-injury research. It encompasses not just basic science and drug development but diagnostics, sporting equipment, and nonpharmacological therapies. At least six organizations—start-ups and university research programs—are now striving to develop concussion drugs. There are efforts to devise an FDA-approved method for diagnosing concussion, including new blood tests, advanced brain scans, and systems that use artificial intelligence to read them. There are newfangled sports helmets. Futuristic materials. Collars that look like chokers and that constrict the jugular to reduce“brain slosh” (a technical term). Hyperbaric oxygen chambers. Visual-oculomotor therapy. The postgame spliff. Out of this field, one group, VanLandingham’s, is trying to create a treatment that eases symptoms and speeds recovery. Another, a start-up helmet maker, is attempting to blunt the head collisions of contact sports, thus possibly saving those sports from a calamitous drop in participation. And a third, in Boston, is testing what it believes could be a cure for the long-term neurological degeneration associated with repeated blows to the head. All address a potential multibillion-dollar market.

Mysteries abide, and VanLandingham has dedicated his life to solving them. “The major thought throughout the history of clinical medicine for concussion has been: There’s nothing to do for it, go lie down, and hopefully you’ll be in the 85 percent of people who get better in a couple of weeks and move on with your life,” he says. “Whereas I’ve always said, Look, if there were a hundred people that fell off a damn ladder today, and 15 of the hundred broke their arm, we’d treat their broken arm! Why the hell aren’t we treating their broken brain? It doesn’t make any fuckin’ sense to me—excuse my language.”

THE SPRAY
THE SHORT HISTORY of modern concussion theory starts in the 1980s, when a neurologist named John Povlishock, Ph.D., at the Virginia Commonwealth University School of Medicine, gave traumatic brain injuries, or TBIs, to animals, euthanized them within hours, and then examined their brains under an electron microscope. Time after time, in the brains of animal after animal, just after an injury, he detected no anatomical change at all. A kind of lag existed, as short as a few minutes, as long as a few hours, before the damage from the injury could be observed. This suggested a window of opportunity. If you acted fast enough, maybe you could interrupt the cascade of neural damage that would eventually set in. Maybe you could intervene.
Povlishock’s findings unleashed a surge of research zeal as scientists sought pharmacological interventions for brain injuries—more than 30 drug candidates went through human trials in the 1990s and early 2000s. In medical circles, their track record remains notorious, a cautionary tale of the scientific method. As James Kelly, M.D., a neurologist and Prevacus advisor, told me, “Every single one of them failed.”
After these high-profile disappointments, research into brain-injury treatments quieted. But the depression didn’t last very long. The signature battlefield injuries in soldiers returning home from Iraq and Afghanistan were, from the beginning, concussions and TBIs of all kinds. Soon the Department of Defense was channeling research dollars to the nation’s neurology departments and public-health institutions. Then, in 2005, the neuropathologist Bennet Omalu, M.D., published the results of an investigation that began with an autopsy of the deceased Pittsburgh Steeler Mike Webster. Webster’s brain, Dr. Omalu found, was plagued with tau proteins, a defining characteristic of chronic traumatic encephalopathy, CTE, the progressive degenerative brain disease that many (but not all) scientists believe results from repeated blows to the head.

Around the time of Dr. Omalu’s discovery, VanLandingham was doing his postdoctoral research at Emory University, and he knew a little about concussions. As a junior at Florida High in Tallahassee in 1991, he was the star quarterback. He could throw a spiral 70 yards and run the 40 in 4.5 seconds. Recruiters from many college programs were courting him, including the hometown Florida State University Seminoles. Then came a series of injuries—a broken sternum, shattered bones in his right (throwing) hand, and, yes, multiple concussions—that effectively ended his football career. After a stint at Division II Valdosta State, in Georgia, stuck on the fourth string, he moved on from the sport and transferred home to Florida State, where he majored in biology.
At around 10:00 p.m. on August 5, 1995, VanLandingham stepped out of a bar in Gainesville, Florida, and took a sucker punch. The fist hit his jaw; his head hit the curb; three blood vessels burst inside his head. The result was a near-death experience. A day later, in the hospital, a hematoma swelled against his cranium. He received a drug, called Decadron, that was in human clinical trials—one of the therapies, post-Povlishock, that ultimately failed to prove itself effective in thousands of other TBI patients. But in VanLandingham, Decadron worked. The pressure normalized; the swelling subsided. “It saved my life,” he says.
Both stories are now integral parts of the Prevacus narrative: The jock turned geek. Personal experience with brain trauma leads to a scientific obsession with finding a cure for TBI. But, VanLandingham tells me, “I didn’t get involved in this because I had a dang brain injury. It’s a sexy story. But I love neuroscience; I’m fascinated by the science of the stuff.”
After he recovered, he graduated from physical-therapy school and worked with brain-injured children for three years. In 2000, VanLandingham left his job as a physical therapist and started pursuing a doctorate in neuroscience at Florida State. In 2004, he began his postdoctoral research at Emory under a renowned neurologist named Donald Stein, Ph.D., whose work focused on the role of a steroid hormone called progesterone, which is crucial to the growth of brain cells. Stein had discovered that rats given brain injuries while their progesterone levels were high recovered from those injuries almost entirely, and he spent decades trying to determine whether progesterone could reduce deadly swelling in the human brain.
While working in Stein’s lab, VanLandingham took the lead in studying the enantiomer, or mirror image, of the progesterone molecule. He and his colleagues found that progesterone’s enantiomer performed just as well as its mirror image in returning rats to cognitive normalcy, and it was better at neutralizing the free oxygen radicals that appear after head injuries and can damage brain cells. If VanLandingham has ever had a eureka moment in his career, this was probably it. “It was clear-cut data. It was beautiful, consistent,” he says. “Those are the most convincing results I ever saw.”
VanLandingham left Emory and took a job as an assistant professor at the medical school at Florida State. But the possibilities of the enantiomer had lodged in his mind. In the late 2000s, with concussions in the news, he began to wonder: Why couldn’t this molecule become a drug that treats people who’ve suffered a concussion? He founded his company in 2012, naming it Prevacus, based on the phrase “prevent a concussion.”
So began years of petri-dish and animal studies. A consultant he’d hired to advise him on FDA regulations suggested that the drug would be faster and more effective in the brain if it were administered nasally, like the anti-opioid-overdose spray Narcan. VanLandingham agreed and worked the nasal spray into his animal trials. All this testing cost money. Here and there, he found it. Perhaps no investor was more important than the wealthy retiree he went to meet one day in 2014 at the office of the retiree’s agent in Hattiesburg, Mississippi.
“I believe in what he’s doing so much that I’ve invested almost a million dollars of my own money,” says Brett Favre over the phone. From that first meeting, he and VanLandingham hit it off. With his own quarterbacking history, his own brain-injury history, and his own laconic southern drawl, Favre was primed to see eye to eye with the person pitching him. “He was a good salesman,” the Hall of Famer says. For a time, they both had high hopes that Favre could help extract some kind of NFL support for Prevacus, preferably financial. “I all but guaranteed him that I could get the NFL on board,” Favre says ruefully. “Boy, was I wrong.” Favre approached executives at the highest levels of the NFL. “But I was politely blown off.” Who did he talk to? “Roger,” he says, not needing to add the man’s surname, which is Goodell. Favre has also approached a few current players—Tom Brady, for example, who was, according to Favre, intrigued.
At one point, Prevacus appeared to be on the verge of human trials. VanLandingham had good reason to believe funding was in place from a Silicon Valley investment firm; Prevacus even issued a press release promising the launch of Phase 1 in the “first half” of 2017. But 2017 came and went with no clinical trial. In the end, the Palo Alto firm never went through with the deal.
Since I began talking to VanLandingham more than a year ago, his target date for the start of Phase 1 trials has kept slipping into the future. At press time, he told me they were likely to start by January. Both he and Favre have been vexed by these delays, and by the trouble in raising money, especially in light of what they view as the excessive focus on funneling research funds to competing technologies. “Stop putting it in helmets!” Favre exclaims during our phone call. “Most of the money now goes to helmet companies,” VanLandingham says. “That’s the disgrace of this shit.” Later he adds, “Vicis is the helmet company that’s getting all the damn money.”

THE HELMET
"ABOUT $85 MILLION since inception,” says Dave Marver, the CEO of Vicis, sitting in his office in Seattle. (Several weeks after reporting this story, Marver stepped down from his role.) That’s the amount of money the start-up has raised in total from the time its founders—the neurosurgeon Sam Browd, M.D., Ph.D., the mechanical engineer Per Reinhall, Ph.D., and Marver—got together in 2013 with the idea of designing a helmet that would revolutionize head protection in football. So far, according to Marver, Vicis’s funding has come chiefly from individual rich people, including NFL stars Russell Wilson and Aaron Rodgers, as well as several owners of professional sports franchises.

One piece of funding in particular was essential to launching Vicis. In 2015, two years before the company brought out its first helmet, it won the GE, Under Armour, and NFL–sponsored Head Health Challenge, a kind of open call by the league for TBI preventative and diagnostic advancements, including helmet technology, part of an overall $60 million investment. With its victory, Vicis received $1.1 million in NFL grant money, a vital bit of not just funding but promotion. “It helped us raise investment capital and get access to NFL locker rooms,” Marver says.
Vicis has spent most of that $85 million on research and development. The company’s executives are fond of noting that Vicis has more engineers on staff, 30, “than the rest of the helmet industry combined.” In the open-plan engineering room, situated in a building in the shadow of the Space Needle, some engineers today are working on the next-gen Vicis helmet, the Zero2. Others are working on top-secret things that the VP of marketing, who is standing next to Marver, is nervous that I might divulge. The company wants to explore other contact sports and helmeted recreations: hockey, lacrosse, cycling, soccer. A helmet for soccer? What could that be? A sophisticated headband? Some kind of water-polo-inspired scalp girdle? The VP looks at me: “I think we’ve teased that as much as we’re going to tease that.”
“Rough day out there,” says Dr. Browd, who has arrived at Vicis headquarters from the operating theater at Seattle Children’s Hospital. It turns out he’s not talking about the successful brain surgery he just performed on a five-year-old child but about the traffic. Dr. Browd is a pediatric neurosurgeon, and over the years, local high school football stars have presented at his office with their third or fourth or fifth concussions. Frequently, his clinical opinion was that those players should never play football again. “You start to have that conversation and everyone in the room is crying,” he says. “It was a conversation I didn’t want to continue to have.”
In 2013, Dr. Browd became one of the NFL’s new independent neurosurgeons, who stand on the sidelines during games and evaluate players for concussion. (He still works Seahawks home games.) He could see firsthand the velocity of the impacts, the damage being done, and, he says, helmet technology that was “really antiquated.” That same year, Dr. Browd drew some ideas literally on a napkin. He then went to Reinhall, head of the University of Washington’s Boeing Advanced Research Center. Two weeks later, Marver met with Dr. Browd and became involved. Far more than his jottings, what Dr. Browd brought to the table was an understanding of the forces that cause concussion. “I said: ‘Look, the medical literature is showing that we think concussions are more likely to come from rotational forces than direct linear impact,’ ” Dr. Browd recalls. “ ‘If we just started from zero, how would you better mitigate that type of force?’ ” Out of these insights came Vicis’s core innovation: a “columnar structure,” a kind of latticework, under an outer shell that deforms upon impact, an idea taken from automotive safety, à la car crumple zones. The columnar structure, too, is designed to absorb and then dissipate the rotational and linear forces of hits in football. Brainstorming this stuff, they felt as though they were injecting some STEM into a stagnant industry. Vicis is Latin for “change.”
Inside a converted garage at Vicis headquarters, the company has created what it calls its “Smash Lab.” The principal pieces of equipment here are machines that bash helmets with pneumatic rams. Resting serenely in front of a pneumatic ram is a crash-test dummy’s head wearing a Vicis helmet. The head is attached to an articulating neck, and the helmet is coated with sensors. An engineer counts down. “Three, two, one . . .” Boom! The head snaps—whiplashed. The word I write in my notebook is “cannon.” A live person standing there with a naked head would, it seems clear, have been killed by that thing. The speed setting for this particular shot, according to the engineer operating it, is 7.4 meters per second—about 16.6 miles per hour. It’s below 9.3 meters per second, which the NFL has determined is the average closing speed of two NFL players in a “concussive or significant” head-to-head impact.

Vicis’s helmet reduces head-impact severity significantly enough to have ranked it number one among all helmets tested by the NFL since it came to market in 2017. But the league only began releasing player-concussion data in 2012, so the sample sizes are too small for any kind of conclusion about concussion reduction. In the lower echelons of the sport—high school, college—there has been little research, and thus limited data, and therefore no evidence on which any helmet maker could base a claim that its headgear reduces the incidence of concussion. And Vicis is very careful about this. They want you to be clear: The company cannot say that its helmets prevent concussions. Its pitch is that its helmet does a better job of “mitigating impact forces.” “Those are hard studies to do,” says Dr. Browd. To do one would require a long-term randomized trial with different helmets, controlled for myriad player-specific variables. It could cost $40 million, he estimates, and “probably needs to happen at the level of the NIH.”
Helmet skeptics aren’t buying it. “To me, the millions the NFL put into helmets is primarily a PR maneuver to make people believe the problem could be solved by helmets,” says Chris Nowinski, Ph.D., a cofounder of the Concussion Legacy Foundation and a former Harvard defensive lineman. “Solving the concussion problem doesn’t necessarily solve the CTE problem.”

THE ANTIBODY
KUN PING LU, M.D., Ph.D., grew up on a rice farm amid the green terraced paddies of rural Fujian Province, in southeast China. Disciplined, focused, he eventually left the countryside for the city, where he earned a medical degree and a master’s degree in pharmacology. After publishing studies on the mechanics of human cell biology, he was recruited to join the Ph.D. biology program at Baylor College of Medicine in Houston. He went there with his young bride, Xiao Zhen Zhou, M.D., who was starting a research position at the University of Texas. She had also grown up on a rice farm and had also earned a medical degree. The year was 1989, the year of Tiananmen Square. Within a decade they had landed on the faculty of Harvard Medical School.
Soon enough, the couple’s research interests converged, first on cancer and then on the brain. In the 1990s, Dr. Lu helped discover a new kind of enzyme, dubbed Pin1, that plays a crucial role in cell division. Through years of lab studies, they learned that an important function of the Pin1 enzyme is to keep a certain set of proteins in their correct shape. Among them is a protein called tau, and tau’s function, in turn, is to build and maintain the brain’s axons, the long tracks of matter that transfer impulses between neurons. Their work suggested that when Pin1 levels are too low, the tau protein deforms. This misshapen version of tau is called cis tau—“the bad guy,” Dr. Lu says. When too much cis tau is present in the brain, axons will break down and collapse. This, according to his theory, contributes to Alzheimer’s disease.
In her earlier work on Alzheimer’s, Dr. Zhou had created a kind of antibody that could detect only the odd shape of cis tau. Using this antibody, she, her husband, and their colleagues observed that cis tau levels in the axons of mouse and human brains escalate sharply in the hours after a single instance of head trauma—whether a mild concussion given to a mouse or a fatal injury such as in a car accident—which they discovered by dissecting victims’ postmortem brains. After repeated mild blows similar to those in sports-
related injuries, or even a single severe head injury or high-pressure blast exposure, as in a traffic collision or a bomb blast, however, the cis tau levels did not return to normal. Through a series of lab studies, the doctors would eventually show the antibody eradicating the bad guy—results that were published in Nature in 2015. Molecularly, behaviorally, cognitively, mice with the rodent equivalent of CTE had been cured.

Kun Ping Lu is a tiny man with graying hair who is quick to laugh. Xiao Zhen Zhou is a tiny woman with graying hair who is quick to laugh. On a day in July, deep inside Beth Israel Deaconess Medical Center, one of the giant Boston research hospitals affiliated with Harvard, the husband-and-wife team, both in their 50s, showed me around their cluttered lab, with its warren of benches, its white-coated young researchers standing at the benches, its computerized time-lapse microscope-imaging systems, its in-vitro neuron-stretching contraptions, its comically gigantic beakers, its cryogenic vats of living antibody-producing cells frozen at –195 degrees Celsius.
Among their most important tasks now is to humanize the antibody—to create a version that can be injected safely into human beings. Dr. Zhou is in charge of the process. It is incredibly painstaking work, almost artisanal. Generations of cell cultures must be nurtured and evolved into further generations with antibody protein sequences ever more humanlike. It is also costly. But no problem. They have NIH/National Institute of Neurological Disorders and Stroke funding. They’ve also cofounded a start-up, called Pinteon Therapeutics, with the goal of eventually commercializing the antibody. Working in parallel with but separate from Dr. Lu and Dr. Zhou, Pinteon’s scientists recently completed the humanization of one variant of the antibody. Pinteon started Phase 1 trials in humans for that variant in September.

Dr. Lu and Dr. Zhou have also been helped along by money from the NFL. Their cis tau antibody is one of four potential treatments for TBI-linked ailments that have received a portion of a $14.7 million grant from the league. Part of the grant, awarded in November 2018, will also fund an epidemiological study that will closely track the changing health, especially in the brain, of as many as 2,500 retired NFL players as they move through the rest of their lives. Bill Meehan, M.D., a brain researcher at Boston Children’s Hospital, who is overseeing the studies, says his group will then select whichever of the four therapies “look most promising in the lab” and bring them into human clinical trials. The idea is to enroll those same retired NFL players as the trials’ subjects. Dr. Meehan will not assess the odds of the four therapies’ success. “But I will say this: The cis tau antibody is very, very far along. I think it’s probably one of the most promising therapies out there.”
Dr. Lu and Dr. Zhou would also like to use the NFL study to understand why many football players who have endured long careers taking repeated head blows never develop CTE. They believe such people may possess a naturally occurring version of their cis antibody, an autoantibody. In other words, they believe there are people who are immune to CTE. To find out, the couple want to examine the retired NFL players enrolled in Dr. Meehan’s study. If they find an autoantibody, they’ll clone it.
Already, Dr. Lu says, “we’re in process of identifying” such players. His voice rises with excitement as he says this. He laughs. But then Dr. Zhou shuts him up. Say no more, her body language commands. The stakes are too high, the work preliminary. “It’s too early!” she says.

DR. LU TOLD ME, “If a player gets a big hit or many small hits, I would give him a dose of the antibody. If it’s caught early, then maybe their sport will not be afraid anymore.” But should any treatment for concussion or CTE ever reach the market, some in the world of concussion science and therapy worry that it might cause other sorts of problems.
“In theory, if it helps the patient recover and doesn’t put them at more risk, it’s a good thing,” says Nowinski of the Concussion Legacy Foundation. “The obvious concern would be: Does it mask symptoms? Does it improve the brain in some ways but not enough to shorten the safe return-to-play window? It has an obvious risk of being abused in a sports setting.”
The concern is part clinical and part cultural. Would a concussion drug or even a CTE cure preserve not only the sport of American football but also its violence? If such treatments exist, do you give the sport license to re-up its commitment to brutality? As Jay Clugston, M.D., a team physician at the University of Florida, puts it to me, a player might say to himself, “It doesn’t matter, man. I’ll lower my head, use my head. I know I can clear up any damage I accrue.”
“As a team physician,” continues Dr. Clugston, who has advised Prevacus, “I gotta say, we’d much rather prevent concussion than we would treat it. If the injury is going to occur, then finding a way to treat it is very important. But I feel like . . . why are we doing this activity if you have to take a drug to protect your brain ahead of time?”
Football’s concussion predicament has long been on VanLandingham’s mind. “You have to first ask yourself: Is football gonna go away if there’s not a treatment? And the answer most likely is no,” he says. But he also once told me, speaking of the Prevacus drug, “I hope one day that this helps keep football . . . as pristine as possible. I love to see a big hit. I think football should be violent. If there wasn’t football, I’d be miserable. It is my favorite thing on this earth.”
You Might Also Like

