Insulin $35 cap price now in effect, lowering costs for many Americans with diabetes
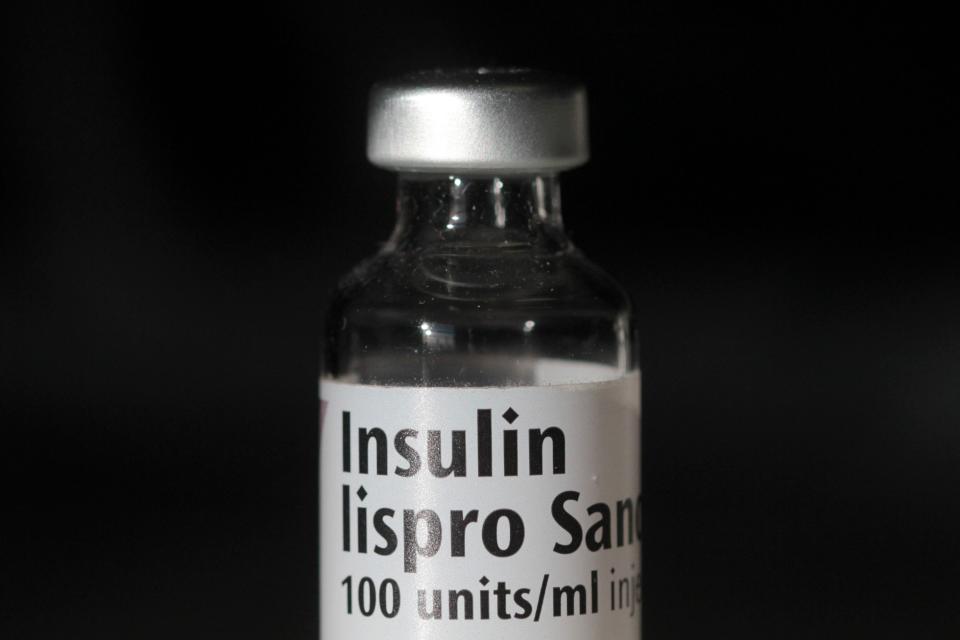
A price cap on insulin from one of the three major manufacturers took effect on New Year's Day, giving more Americans with diabetes more affordable treatments.
In March, Sanofi became the last of three companies that make up 90% of the world's insulin market by value to announce price cuts. Novo Nordisk and Eli Lilly Co.'s plans had slashed U.S. prices by up to 75% and 70%, respectively.
As of Jan. 1, 2024, Sanofi cut the price of Lantus by 78% and short-acting Apidra by 70%.
The price cuts will reduce the cost of the drug for most patients at $35 through either price caps or savings programs.
The Paris-based pharmaceutical company said earlier that most people with private insurance already pay $15 or less because of a copay assistance program. The drugmaker's program for the uninsured also offers a 30-day supply for $35.
Analysts, politicians and patient advocates have increasingly criticized drug manufacturers for the prices set for insulin. In recent years, federal and state laws, Medicare and Medicaid policies, and changing market dynamics for these older insulin drugs have influenced price cuts.
But more needs to be done, said Elizabeth Pfiester, founder and executive director of T1International, an advocacy organization for people with Type 1 diabetes.
Millions of people need the lifesaving medication. According to the American Diabetes Association, spending on insulin has tripled in the past decade to $22.3 billion in 2022, and the inflation-adjusted cost of the drug increased 24% between 2017 and 2022.
A 2020 survey from the Pfiester organization found that 1 in 4 people with Type 1 diabetes rationed insulin because of cost. Patients also struggled to pay out-of-pocket for other supplies such as insulin pumps, testing strips and continuous glucose monitors.

Lower drug costs: 3 major insulin makers have now slashed the price of the life-saving drug. Here's why.
Your life in data: Explore our tool that shows what pharmacies pay for prescription drugs
Why is insulin so expensive?
Insulin prices charged by the three major drug manufacturers spiked over the past two decades. From 2002 through 2013, the average price of insulin nearly tripled, according to the American Diabetes Association.
A Senate Finance Committee investigation in 2021 found the drug price increases coincided with lucrative rebate demands from insurers and pharmacy benefit managers, which are drug-pricing middlemen that command steep rebates in exchange for favorable placement on private insurance plan drug formularies.
In the past decade, these pharmacy managers began to pit manufacturers against one another by excluding them from large blocks of patients through formulary exclusions, the Senate Finance Committee reported.
Why insulin prices are starting to drop now
In 2022, a sweeping climate and health bill called the Inflation Reduction Act capped insulin costs at $35 a month for Medicare enrollees. In February 2023, Biden urged Congress to extend that out-of-pocket cap to younger Americans with private health insurance.
Washington, D.C., and 22 states have enacted cost-sharing limits for consumers purchasing insulin, according to the American Diabetes Association.
Drugmakers also are bracing for a drug pricing change under Medicaid, the federal health program for low-income families. Medicaid has required drug companies to pay rebates when they significantly raise prices over time. However, the amount drug companies paid Medicaid was capped in previous years.
The new provision, part of the American Rescue Plan Act passed in 2021, eliminates the rebate cap beginning next year. In other words, drug companies could face significant financial penalties starting this year, said Antonio Ciaccia, CEO of 46brooklyn Research, a nonprofit that researches drug pricing.
The elimination of this Medicaid rebate cap, in particular, might be influencing drugmakers' decisions to drastically cut insulin list prices, Ciaccia said.
"It's one thing for a drug manufacturer to offer something for free," Ciaccia said. "It's another thing to literally pay for the privilege of doing so."
This article originally appeared on USA TODAY: Insulin price cap: More Americans will now pay no more than $35

