What Is Insulin Sensitivity?
How to treat sensitivity and resistance to insulin
Medically reviewed by Kelly Wood, MD
Insulin resistance indicates that your body struggles to manage your blood sugar levels. Left untreated, this can lead to several health problems, including type 2 diabetes. But how can you tell whether you have insulin resistance, and what can you do to improve insulin sensitivity?
This article examines insulin sensitivity, including factors involved, potential symptoms, and how to manage it to reduce your risk of developing type 2 diabetes.
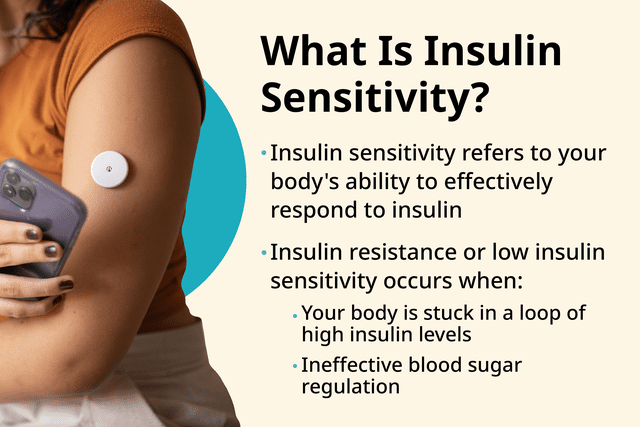
Photo composite by Michela Buttignol for Verywell Health; Getty Images
Defining Insulin Sensitivity and Role in Metabolism
Insulin sensitivity refers to your body's ability to effectively respond to insulin, an essential hormone in regulating blood sugar levels.
When you eat, your body digests carbohydrates into glucose (sugar) molecules, which enter your bloodstream. To lower your blood sugar, your pancreas—an organ that supports digestion and hormones—releases insulin. The insulin travels to your blood, where it helps move sugar molecules into your cells. From there, sugar is transported to tissues and organs throughout your body, which it can use for energy. This results in lowered blood sugar.
This process is critical for keeping your blood sugar levels within a healthy range. However, when you have insulin resistance, your cells become less responsive to insulin signals, impairing the process of moving sugar from blood to cells. In other words, sugar molecules remain in the blood longer than they should, prolonging high blood sugar levels.
As a result, the pancreas tries to compensate by producing more insulin to lower blood sugar, but this ends up causing high insulin levels in the bloodstream.
Insulin resistance or low insulin sensitivity occurs when your body is stuck in a loop of high insulin levels and ineffective blood sugar regulation. Over time, this can contribute to a higher risk of type 2 diabetes, heart-related problems, and other health complications.
Related: What Is Insulin?
Low vs. High Insulin Sensitivity
Low insulin sensitivity is when your cells have a reduced response to insulin, leading to impaired glucose uptake, higher insulin levels in the blood, and an increased risk of metabolic disorders like type 2 diabetes.
High insulin sensitivity is when your cells respond normally to insulin, facilitating glucose uptake, keeping your blood sugar levels stable, and reducing the risk of health complications.
Factors Affecting Insulin Sensitivity
Many factors, including genetics, lifestyle, and medical conditions, can influence insulin sensitivity. Some common factors that can play a role include:
Genetics: Having a genetic predisposition (for instance, if your parent or grandparent has insulin resistance) can influence how effectively cells respond to insulin signals further down the family line.
Body composition: Excess body fat, particularly around the abdomen, is associated with reduced insulin sensitivity.
Physical activity: Regular exercise supports insulin sensitivity by promoting glucose uptake in muscles and improving overall metabolic health.
Nutrition: Dietary factors like the quality and balance of carbohydrates, fats, and proteins can impact insulin sensitivity. Ultra-processed foods high in saturated fat, sodium, and added sugar tend to be low in nutrients and can promote insulin resistance.
Sleep: Poor sleep is linked to decreased insulin sensitivity and an increased risk of insulin resistance.
Stress: Chronic stress can keep levels of cortisol ("the stress hormone") high, impairing insulin sensitivity and contributing to insulin resistance.
Hormonal imbalances: Hormones like cortisol, growth hormone, and thyroid hormones, as well as hormone-related conditions like polycystic ovary syndrome (PCOS), can influence insulin sensitivity.
Medications: Certain medications, such as corticosteroids, can decrease insulin sensitivity.
Age: Insulin sensitivity tends to decline with age, partly due to changes in body composition and hormonal fluctuations.
Environmental factors: Pollutants, like endocrine-disrupting chemicals, may impact insulin sensitivity.
Related: Hyperinsulinema (High Insulin Levels)
Symptoms of Low Insulin Sensitivity
Symptoms of low insulin sensitivity or diabetes can show up in many ways, such as:
Ongoing fatigue and low energy levels
Increased thirst
Having to use the restroom more frequently
Increased hunger and cravings for sugary or carbohydrate-rich foods
Trouble losing weight despite efforts
Brain fog or difficulty concentrating
Dark patches on your skin, called acanthosis nigricans, especially in the armpits, groin, or around the neck
Irregular menstrual cycles
Increased blood pressure
If you're experiencing any of these symptoms or have concerns about your metabolic health, speak with a healthcare provider. Left untreated, insulin resistance poses significant health risks.
It increases the likelihood of developing type 2 diabetes as your pancreas struggles to produce enough insulin to overcome cellular resistance. It also increases your risk of cardiovascular diseases such as heart attacks and strokes. Insulin resistance is also linked to obesity and various metabolic disorders like nonalcoholic fatty liver disease and PCOS.
Signs in Someone Else
It can be easier to recognize signs of health problems in someone else than in yourself. If you notice physical symptoms in someone that may indicate insulin resistance, such as dark skin patches or changes in their appetite or bathroom habits, bring it to their attention lovingly and respectfully. Many people are unaware that they have insulin resistance or are on their way to developing type 2 diabetes.
Do I Have Low Insulin Sensitivity?
The only way to know if you have low insulin sensitivity is to see a healthcare provider for a diagnosis. In addition to a comprehensive physical exam, they will likely order tests to measure the glucose and insulin in your blood at various points of the day.
Fasting Insulin
Fasting insulin levels (meaning you haven't eaten in at least eight to 12 hours) are measured after an overnight fast (sleeping) to evaluate how much insulin your body produces at baseline. Normal fasting insulin levels for individuals without diabetes typically range between 2 and 25 micro international units per milliliter (µIU/mL), but this can vary.
Glucose Tolerance Tests
Glucose tolerance tests involve measuring blood sugar levels before and after consuming a standardized glucose solution to assess how effectively the body clears glucose from the bloodstream.
Normal fasting blood sugar levels are generally less than 100 milligrams per deciliter (mg/dL). Normal blood sugar two hours after consuming a meal (or a glucose solution in a glucose tolerance test) is typically less than 140 mg/dL.
Other Blood Markers
Sometimes, providers want additional markers of insulin sensitivity that can be measured with tests called the homeostatic model assessment for insulin resistance (HOMA-IR) or the quantitative insulin-sensitivity check index (QUICKI). These use calculations based on fasting glucose and insulin levels to estimate insulin sensitivity.
Higher fasting insulin levels, impaired glucose tolerance, and elevated HOMA-IR or reduced QUICKI scores indicate low insulin sensitivity and may suggest an increased risk of type 2 diabetes. Lower fasting insulin levels, standard glucose tolerance, and lower HOMA-IR or high QUICKI scores suggest better insulin sensitivity and metabolic health.
Related: Insulin Resistance: How to Test and Manage Symptoms
Managing Insulin Sensitivity Through Self-Care
Your everyday lifestyle habits have the most significant impact on your insulin sensitivity. Taking care of your physical and mental well-being is essential for your overall health. Still, the positive effects of this also trickle into details like your body's ability to manage glucose and insulin.
Some of the best self-care habits for insulin sensitivity include:
Regular physical activity: Include a variety of movements, like jogging, swimming, biking, and strength training. Exercise improves insulin sensitivity by enhancing glucose uptake in muscles and reducing insulin resistance.
A nutrient-rich diet: Mainly eating whole foods that provide fiber, protein, and healthy fats while limiting ultra-processed items can help stabilize blood sugar levels and support insulin sensitivity.
Sleep and stress management: Experts recommend adults get seven to nine hours of sleep per night. Getting adequate sleep and practicing stress management techniques like journaling, taking a nature walk, listening to calming music, or meditating can help support your metabolic health.
It's also essential to have regular wellness exams, especially if your provider determines that you're at risk for insulin resistance or diabetes. Follow their recommendations, which may include blood sugar monitoring.
Related: How Do Different Types of Insulin Work?
How to Medically Treat Insulin Sensitivity
Medically treating insulin sensitivity often involves a combination of lifestyle modifications and medications to improve glucose regulation and metabolic health.
Commonly prescribed medications for insulin resistance can include:
Metformin
Thiazolidinediones
DPP-4 inhibitors
GLP-1 receptor agonists
SGLT2 inhibitors
Each of these medications has its own set of potential side effects. Some of these include digestive upset, unwanted weight gain, fluid retention, and an increased risk of heart failure.
In cases of severe insulin resistance or type 2 diabetes, insulin injections may also be necessary to supplement your natural insulin production and improve blood sugar management.
Work with your healthcare provider to determine whether you need medical intervention for insulin sensitivity.
Tips for People With Increased Risk Factors
The best thing you can do if you're at an increased risk of insulin resistance or type 2 diabetes is to be proactive. Identify areas where you can make lifestyle adjustments to support your overall health better.
If you already have diabetes, manage it as directed by your healthcare provider to keep your blood sugar and insulin levels within a healthy range. Consider what you can do to achieve and maintain a healthy weight, engage in regular physical activity, and fuel your body with nutrient-rich, minimally processed foods.
Get regular wellness exams and communicate with your provider should any questions, concerns, or changes in your health arise.
Summary
If you're struggling with insulin resistance, you're not alone. You should feel empowered by the many things you can do to improve your insulin sensitivity and overall well-being. Everyday lifestyle habits like a nutrient-rich diet, regular exercise, and adequate sleep can support healthy weight and blood sugar management. Speak with a healthcare provider if you're concerned about your insulin sensitivity because they can provide individualized guidance or recommend a dietitian or certified diabetes educator.
Read the original article on Verywell Health.

