New Jersey's goal is to saturate the state with naloxone to save lives
Officials across New Jersey are on a mission to saturate the state with a potentially lifesaving medication.
Now available for free at select pharmacies statewide, the opioid-blocking drug naloxone can revive the lifeless from an overdose in seconds. It is not something many expect to use. Still, like a fire extinguisher, it can be lifesaving in an emergency, said Nina Cooperman, a faculty member at Rutgers University's Robert Wood Johnson Medical School who oversees the state's Opioid Overdose Prevention Network.
"You never know, whether it's a family member or a friend or just a stranger walking down the street," Cooperman said.
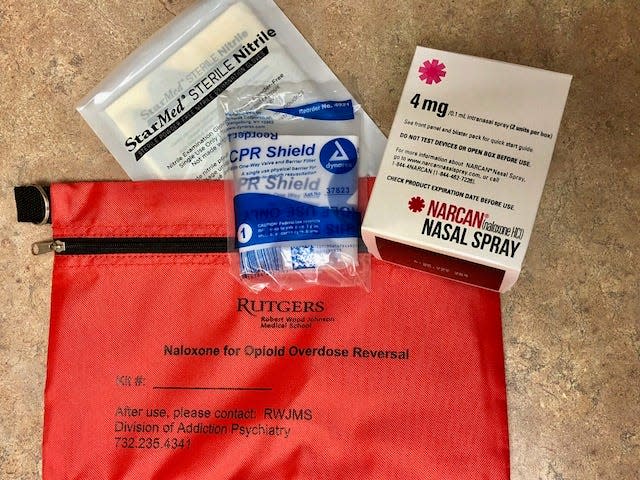
Cooperman and her team of health educators at the network said it is their collective mission to distribute naloxone and training on how to use it to as many people as possible. They get support from the state's Division of Mental Health and Addiction Services and the university's Division of Addiction Psychiatry.
Story continues below map of locations where naloxone can be found.
Ideally, naloxone should be a part of any first aid kit, Cooperman said. At airports, schools and other places where people congregate, adding naloxone to an emergency response toolkit has gained traction. Now, the aim is to get the opioid blocker into homes, pockets and purses.
Free naloxone
Since January 2023, anyone 14 or older can request and obtain naloxone for free from participating New Jersey pharmacies. Recipients do not need to provide a prescription, a name or a reason. Pharmacies can offer one two-dose nasal spray kit per visit.
Developed by the state Department of Human Services in partnership with the New Jersey Board of Pharmacy and its Medicaid division, the state's nearly year-old Naloxone365 program reimburses pharmacies for each naloxone kit. Pharmacies source the naloxone and bill the state at the Medicaid rate.
Three dozen Bergen County pharmacies participate in the program, including leading chains and locally owned shops, according to state records. There are 43 more in Passaic County and 33 in Morris County. Statewide, there are more than 600 participating pharmacies. A list can be found at StopOverdoses.nj.gov.
From January through August 2023, state officials tallied 10,184 uses of naloxone by law enforcement and other emergency responders, the state Attorney General's Office said. During that same period, they counted more than 2.13 million dispensed opioid prescriptions. Then there are the street drugs.
Opioid overdoses
Lt. Robert Bracken, a detective with the Clifton Police Department, said the force sees an overdose from street drugs once a week at minimum.
According to records kept by the Opioid Overdose Prevention Network, a 2022 study found that supplies of street heroin in New Jersey were far more likely to include fentanyl than heroin. Bracken said it is also becoming increasingly common to find fentanyl mixed with street cocaine or in counterfeit versions of Adderall and Xanax, as illicit drug manufacturers seek to increase their profit margins by cutting their product with a relatively cheap but powerful drug.
"Someone could just be using for the first time and overdosing," Cooperman said. "And there are people who are not even intending to use an opioid but inadvertently do."
The overdoses and deaths triggered by fentanyl are hard to track, Bracken said. It is not unusual for six months to pass before a suspected overdose death receives a corresponding toxicology report. Regardless, statistics show that fentanyl overdoses have climbed steadily since 2015 and have, said the state Department of Health, become the state's largest contributor to overdose deaths. While New Jersey's death rate from drug overdose trails the national average, its death rate from opioids and heroin in particular remains above average, shows data compiled by the Centers for Disease Control and Prevention.
Jerry Speziale, Paterson's public safety director, said fentanyl and other more potent forms of opioids are making overdoses more likely — and more likely to overwhelm a typical naloxone dose. Carfentanil, a synthetic opioid not for human use that is about 100 times more potent than fentanyl, is among them. There is also a non-opioid tranquilizer called xylazine, which was found in more than a third of street heroin samples in the 2022 study.
“Sometimes naloxone doesn’t work,” Speziale said. "It can really depend on the timing or how you are administering it," whether by nasal or intramuscular application.
Giving naloxone is at least worth a shot, said Cooperman and others.
"It's not the kind of thing that would harm anyone," Cooperman said. "The only thing is that if someone is overdosing from an opioid, naloxone could not only reverse their overdose, it could put them in a withdrawal."
What is naloxone?
Patented in 1961, naloxone was approved by Food and Drug Administration officials a decade later as a treatment for opioid overdose.
In May 2013, former Gov. Chris Christie signed the Overdose Prevention Act, allowing health care professionals to dispense naloxone to patients and those who "may be in a position to assist another individual during an overdose.” Still, until about 2015, the drug was mostly confined to hospitals and emergency response situations. Then, in November 2015, the FDA approved a device called Narcan Nasal Spray for delivering measured doses of naloxone.
More: Bergen County announces new initiative to stock naloxone kits at its facilities
Cost barriers were an issue. They still can be. Though down from well over $100 per two-dose pack of Narcan, a common brand of naloxone spray, the cost is about $45 at most pharmacies. The spray does not last forever, either. Naloxone products typically have a shelf life of 18 to 24 months if kept cool and dry.
Historically, access to naloxone was limited to community-based distribution programs. However, in 2018, state Department of Human Services officials authorized a standing order allowing permitted pharmacies to dispense naloxone without an individualized prescription. Last year, it launched Naloxone Direct, giving statewide agencies the ability to request direct shipments of naloxone online.
Between 2018 and August 2023, state programs distributed about 270,000 two-dose naloxone kits to individuals and to first responder agencies, harm reduction groups, county prosecutors' offices, libraries and shelters. More than 40,000 of the kits were distributed by pharmacies participating in the Naloxone365 initiative, state records show.
How is naloxone distributed?
Beyond pharmacies, groups such as the Opioid Overdose Prevention Network and the New Jersey Harm Reduction Coalition are mailing free naloxone kits to homes and post office boxes. In a statement, coalition officials said they encourage all individuals to carry naloxone, but at times of limited supply they may prioritize getting naloxone to people most likely to witness an overdose. The coalition offers intramuscular or intranasal naloxone depending on price and availability.
More: The Giants' Darren Waller nearly died of an overdose. Now he helps NJ kids beat addiction
Distributing naloxone is just the start, however. State agencies and other groups offer online training videos to provide instruction on its use. Some experts offer free online community training on how to prevent, recognize and respond to an opioid overdose.
The Opioid Overdose Prevention Network developed by the state Division of Mental Health and Addiction Services in partnership with the Division of Addiction Psychiatry at Rutgers Robert Wood Johnson Medical School offers free education and naloxone. Since its creation in 2017, the network has provided both to more than 18,000 people.
Currently, it offers free public presentations and naloxone distribution events six times a month for those 18 or older, who reside, work or attend school in New Jersey. The sessions are conducted online via Zoom and the kits are distributed via UPS within a week.
Other groups still travel to provide training. In North Jersey, the Morris County Sheriff's Office's Hope One mobile unit — a sheriff’s officer, a licensed mental health professional and a certified peer recovery specialist — helps people access in-person training.
Directions on how to use naloxone
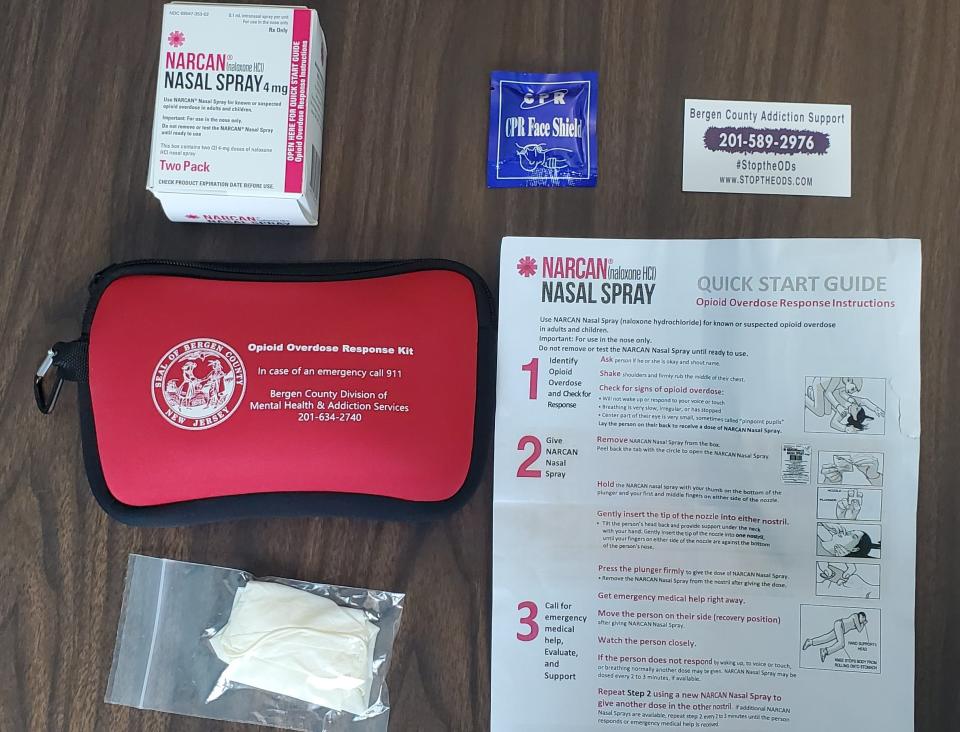
Five steps for naloxone administration:
According to experts, the first thing to do is ask the person suspected of having an opioid overdose if they are OK. Shout their name. Shake them, and check their breathing, complexion, pupils and heartbeat. If they are limp, unable to speak, vomiting or otherwise unresponsive, call 911.
After calling first responders, Opioid Overdose Prevention Network officials recommend using rescue breathing if needed while getting the naloxone out of its packing.
To use the naloxone spray, first tilt the person's head back and support their neck with your hand. Using your other hand, hold the spray with your thumb on the bottom of the plunger and your first and middle fingers on either side of the nozzle. Insert the tip of the nozzle into one nostril until your bent fingers hit their nose. Then, depress the plunger. Have the other spray nearby, as another dose could be required in two to three minutes.
The person suspected of having an overdose may start breathing on their own. If so, roll them onto their left side with their right leg and right arm crossed over their body to keep them stable and prevent choking. Then, wait until help arrives.
If the person does not start breathing or is gasping for air, chest compressions and rescue breathing are recommended until 911 assistance arrives.
This article originally appeared on NorthJersey.com: Should you add naloxone to your first aid kit? Yes, say experts

