These Killer Germs Could Be Lurking In Your Lawn

There’s no shortage of nasty germs in the world that can make us sick. The most common ones tend to be those passed on from person to person through methods such as respiratory droplets and aerosols, fecal-oral contamination (touching traces of poo from someone’s unwashed hands), or even sex. But there are other insidious buggers lurking elsewhere in the environment, including the very soil underneath our feet.
Many of these dirt-loving pathogens primarily call soil their home, and only rarely cause problems when they inadvertently end up in people; others regularly infect people and animals, with their time in soil being one part of their complex life cycle. But they can all potentially cause serious harm when we come into contact with them. Here are some of the dirtiest germs out there.
Read more
These Winning Close-Up Photos Show Life That's Often Overlooked
Remembering Enterprise: The Test Shuttle That Never Flew to Space
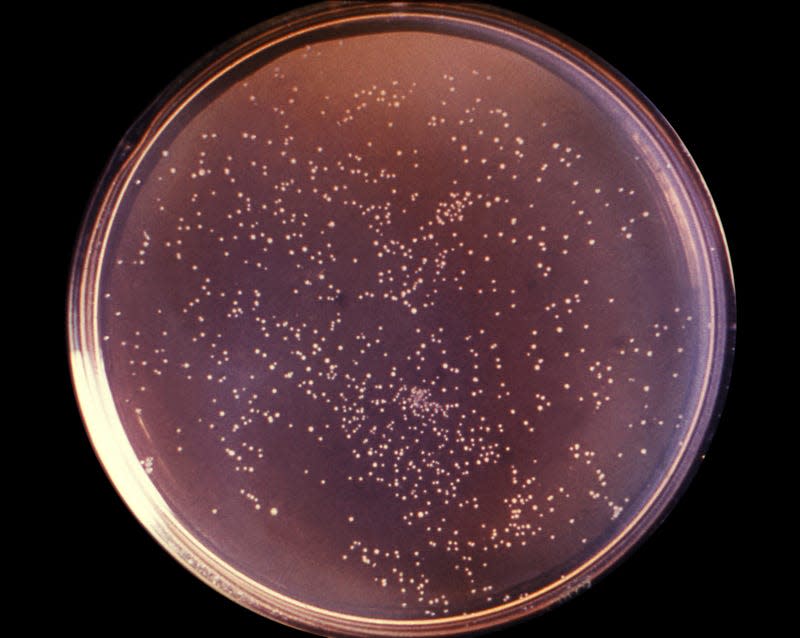
Anthrax

The infection: Anthrax, caused by the bacteria Bacillus anthracis.
Symptoms and treatment: Its symptoms vary depending on how we’re exposed to the bacteria. When it’s inhaled, it’s often highly fatal. Prompt treatment with antibiotics and antitoxins can prevent or treat serious cases, though.
Threat potential: People usually catch anthrax from infected animals or contaminated animal products. But the ubiquitous presence of anthrax spores in soil provides a constant opportunity for the bacteria to jump into animals. Thankfully, many countries, including the U.S., regularly vaccinate their livestock and a vaccine is available for humans at higher risk of exposure, so cases today are rare. Anthrax still remains a potential bioweapon threat, given its ability to be aerosolized.
Leptospirosis

The infection: Leptospirosis, caused by various members of Leptospira bacteria.
Symptoms and treatment: It can initially cause high fever, chills, muscle aches, and jaundice (yellowed skin and eyes). Sometimes, people can recover and later experience a worse and more life-threatening second phase of illness, one that can severely damage the liver, kidneys, and brain. The second phase is more common when the infection goes untreated with antibiotics.
Threat potential: The bacteria is spread through the infected urine of various animals, including rats, which can then end up contaminating nearby sources of water or soil for weeks to months. Though rare in the U.S., there have been recent spikes in places like New York and experts fear that a warmer climate will make cases more common.
Brain-eating amoebas
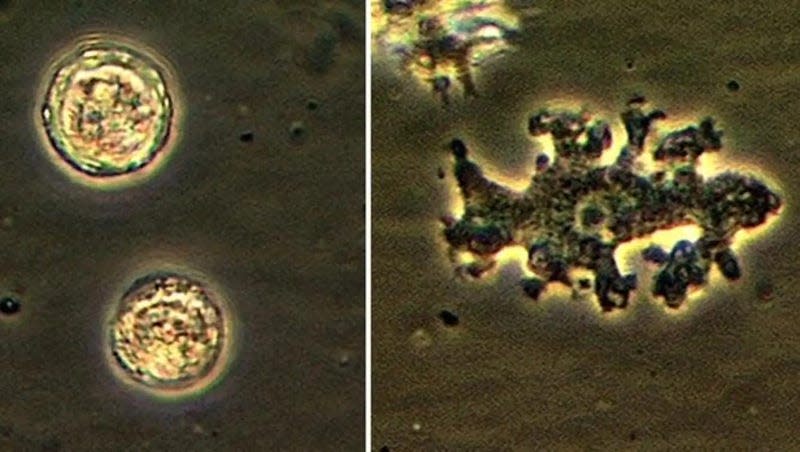
The infection: Primary amoebic meningoencephalitis and granulomatous amebic encephalitis (GAE), caused by various species of free-living amoeba that invade and eat away at the brain.
Symptoms and treatment: Initial neurological symptoms include confusion and loss of coordination, which is often followed by more serious complications like seizures, coma and ultimately death.
Threat potential: These amoebas are abundantly found in soil and water environments, where they normally feast on bacteria. Some species can be a relatively common source of eye infections, but all of them only rarely cause the brain-eating variety. Even so, these latter infections are almost always fatal. And in a few cases, it’s likely that people directly contracted the amoeba from contaminated soil.
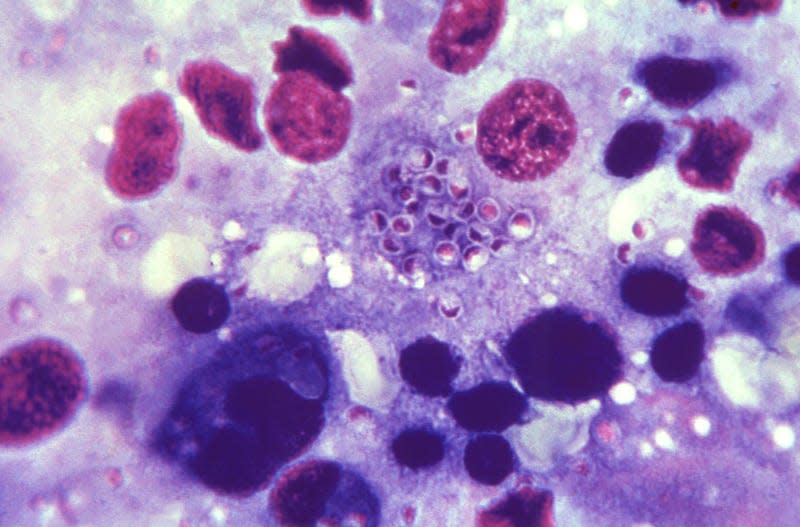
Valley Fever

The infection: Valley fever, caused by the fungus Coccidioides.
Symptoms and treatment: Its symptoms are similar to many respiratory illnesses and include fever, cough, and headaches. About 5% to 10% will go on to have serious long term lung problems, and a smaller percentage can develop life-threatening complications.
Threat potential: The fungus lives in the soils of the southwestern United States, parts of Mexico and Central America, and parts of South America. Though most people exposed to Coccidioides don’t become sick, cases of Valley fever have been increasing in recent years. And many experts fear that a rise in dust storms, fueled by climate change, will only make the disease more common and widespread.
Melioidosis
The infection: Melioidosis, caused by the bacteria Burkholderia pseudomallei.
Symptoms and treatment: Symptoms vary, depending on how people are exposed to it. In people with a respiratory infection, for instance, it can cause fever, cough, and headache. Though treatable with antibiotics, its fatality rate can be as high as 50%.
Threat potential: The bacteria is typically found in the soil and waters of tropical environments. But some scientists have warned that a warming climate will allow the bacteria to establish a permanent reservoir in the United States. Just last year, CDC officials confirmed the first outbreak of the disease traced back to the continental U.S.
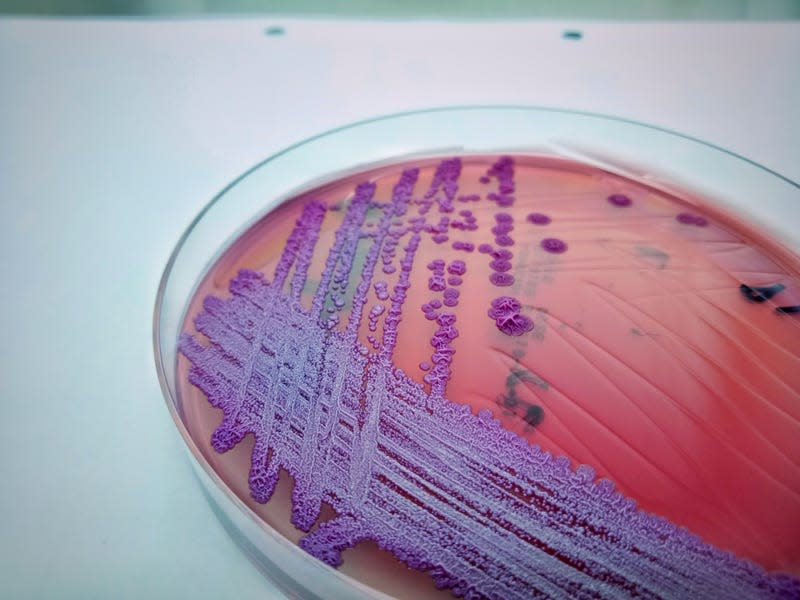
Histoplasmosis
The infection: Histoplasmosis, caused by inhaling the fungus histoplasma. This usually happens when disturbing dirt contaminated with it.
Symptoms and treatment: It can cause fever, cough, fatigue, chills, and aches. In more serious cases, it can cause chronic lung infection or spread elsewhere throughout the body.
Threat potential: Most people who come into contact with histoplasma don’t develop illness, while others will only experience mild symptoms. But it can be dangerous to people with weakened immune systems. And it may be more common than thought. A study last year found that infections have been occurring all throughout the U.S. in recent years, suggesting that the fungus is living in the soils of nearly every state.
Tetanus

The infection: Tetanus, caused by Clostridium tetani bacteria entering the body through an open wound or cut.
Symptoms and treatment: The most common and infamous sign of tetanus is lockjaw, or a tightening of the jaw muscles. Others include sudden muscle spasms, painful stiffness, and trouble swallowing. Sometimes, the involuntary contractions are so brutal that it leads to broken bones. Death tends to happen when people lose the ability to breathe on their own.
Threat potential: Even with antibiotic and antibody treatment, roughly one in ten people die from tetanus infection. And since tetanus spores are everywhere in the soil and surrounding environment, there’s always some risk of infection from getting your skin punctured or tore open outside. Thankfully, there’s a widely available and effective childhood vaccine (and booster in adults) that has dramatically lowered cases and deaths in recent decades. But roughly 37,000 people a year worldwide continue to die from it, and there’s still the occasional case in America too.
Plague
The infection: Plague, caused by the bacteria Yersinia pestis.
Symptoms and treatment: Symptoms vary on the form of infection it takes. The most serious kind is pneumonic plague, which is highly deadly without prompt antibiotic treatment and can be contagious to others.
Threat potential: Plague is responsible for some of the worst pandemics in human history. The availability of antibiotics and improved sanitation (its most common vectors are rodents and their fleas) have made it less of a threat these days, but it still causes periodic outbreaks. Plague bacteria circulate in several animal hosts, but some recent research has suggested that it hides inside soil-loving amoeba as well. And at least some scientists believe that its disappearing act in soil is how the plague has managed to reemerge to wreak havoc time and time again. Climate change may also allow it to become a more common threat in the future.
More from Gizmodo
Sign up for Gizmodo's Newsletter. For the latest news, Facebook, Twitter and Instagram.

