Know how to spot a stroke: BE FAST is the new acronym
When it comes to strokes, every minute it takes a person to get medical help can mean precious resources to the brain are being depleted.
But how do you know when someone is having a stroke? In some cases, it is not obvious.
Our medical expert for Healthy Actions this month is Dr. Susana Bowling, the medical director of the Neuroscience Institute at Summa Health in Akron and Summa’s Comprehensive Stroke Center.
More: Betty Lin-Fisher: Links to Healthy Actions columns
This is an edited version of our interview. Bowling provides valuable information, especially during May, which is National Stroke Awareness Month.
There also is a video and podcast available of our interview.

Can you tell me about your stroke programs at Summa?
I am the director of the Comprehensive Stroke Center at Summa Health System located primarily at Akron City Hospita.l It’s a program that has been dedicated for many years for the care of patients with acute stroke, stroke in general and TIAs (transient ischemic attack). Just recently, we acquired accreditation as a comprehensive stroke center, which means we can not only treat ischemic strokes effectively, but we expand the treatments to hemorrhagic strokes.
Healthy Actions: Oh my aching back! Tips from a spine surgeon
What are some common signs or symptoms of a stroke? What is FAST?
For many years ago, the stroke community had an acronym of FAST. It was something catchy and easy to remember to help patients and community members to know the symptoms of a stroke. "F" is for the face. If there is any drooping or weakness on one side? Can the person smile? "A" is for arms. Do you have a sudden onset of weakness in one arm? "S" is for speech. Are you having difficulty speaking or slurring your words? Are people having a hard time understanding you? "T" is for time to call 911. Time is brain, therefore you need to act very quickly.
What are some other common signs of stroke. And what is BE FAST?
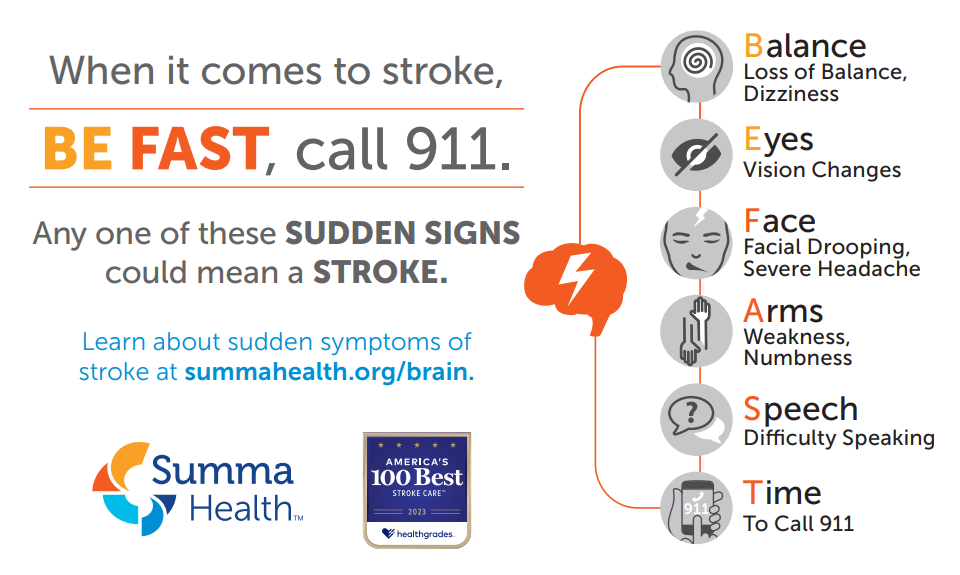
We used the FAST acronym for years until recently. The stroke community wanted to expand the education for the public to know there are other symptoms that could also suggest a stroke. We have now have BE FAST. "B" is for balance. Does the person have a sudden loss of balance? This is not necessarily someone who has balance issues from ear problems or something they already know they have balance issues. This is a sudden loss of gait or balance and the person ends up falling or not. Those patients may not be asking for help in a timely manner. "E" is for eye. Has the person lost vision in one or both eyes?
So to recap:
B is for Balance
E is for Eye
F is for Face
A is for Arm
S is for Speech
T is for Time to call 911
It is impossible to put in one acronym every sign of a stroke, but I would say this represents more than 90% of typical stroke symptoms.
A big sign is sudden onset: you were fine one minute and the next minute, you are not. Some examples are: you wake up with symptoms when you went to bed perfectly normal. You’re talking on the phone and suddenly you lose your speech. All the things that are sudden, no matter where the weakness is, it’s very important to consider as a symptom of a stroke.

Do strokes only happen to older people or men?
People think stroke is a disease of the elderly and it’s not true. Data from Ohio suggests that 60% of strokes are below the age of 65. These are individuals who are still working in the community, providing for their families and having a very beautiful life. Strokes are now affecting a younger population and as time goes along because the typical triggers or risk factors for strokes are becoming more prevalent in the younger population.
For many years, the thought was that strokes occur in men and don’t occur in women. Women have always been more reluctant to ask for help when they have symptoms. They tend to ignore their symptoms.
As a matter of fact, women have more strokes. When it does happen, it tends to be in a little older age range and it tends to have more significant consequences and effects.
Women tend to be the caregivers, not the ones that take the care, so the consequences of having a stroke in women is usually more devastating.
Healthy Actions: Q&A: Have a headache or a migraine? A doctor offers advice
Are you seeing strokes in people in their 20s and even teens?
Yes and there are strokes in children, too. It happens at any age. That can also come with the use of drugs as they increase the chances of having strokes. It comes with the increased prevalence of obesity in youth and with that, the presence of diabetes, hypertension and high cholesterol. All those are risk factors of a stroke at any age.
Are there tips to prevent a stroke?
The No. 1 tip is take care of yourself as a whole. Engage with the care of a physician early on. Having well-visits with primary care physicians. When you have a diagnosis like diabetes, hypertension, high cholesterol — all of those diagnoses don’t hurt, so people don’t run for help because, "Hey, I don't feel my high blood pressure, why should I treat it? I feel perfectly OK."
When you have those diagnoses, you heed to treat those because we call those the silent killers. Be consistent with your treatments because they are chronic conditions and don’t go away. Understand that treatment is going to prevent conditions like a stroke or heart disease, which will change your lifestyle.
What are the types of strokes? What is a TIA?
A TIA, or transient ischemic attack, is what I would consider as a prelude to a stroke. The stroke has not happened, but it's coming. Usually about 17% of patients that had big strokes had a TIA seven days prior to the event. That means you’ve had transient symptoms of the BE FAST acronym. But instead of lasting for over an hour, they tend to be five or 10 minutes and that’s the reason why patients don’t tend to get help because they don’t think it’s serious. "Oh, my arm was weak for 5 minutes, but it’s back to normal. Why would I bother?”
It’s transient and has the same symptoms and goes away before it injures the brain, but it is a prelude to an event that could eventually cause permanent damage.
Healthy Actions: Are you tired? You may need to go to the doctor if it persists | Betty Lin-Fisher
Is there a time frame that is important with strokes?
When symptoms last more than an hour, more than 80% of those patients would have already had a stroke. It takes five minutes for neurons in your brain to start dying. With more accurate and improvements in technology and imagine, we have been able to identify strokes in patients who have had symptoms sometimes for even five to 10 minutes.
If you see any BE FAST symptoms, call 911. If you have any of these symptoms, this is the one chance that life has given you to take actions before you can no longer take an action.
Should you call 911 or drive yourself or have a loved one drive you to the ER?
You need to call 911, particularly in our system. The EMS crews in our communities are extraordinary and very well trained. They know what information to get, but they also know how to treat the patient during transport to the ER. If the patient gets worse during transport, they know what to do. They call us before they come so we are waiting for them.
It facilitates for a patient to be treated faster. A patient’s treatment starts when the first healthcare professional is involved and that is EMS in the home of the patient or where ever they’ve had the stroke.
Healthy Actions: In need of a good night's sleep? Here's tips and help from a doctor| Betty Lin-Fisher
What does 'time is brain' mean?
Every minute counts, so the longer you wait to seek any help, the more deficits you would be accumulating and the worse outcomes you will have. On top of that, the more you wait to come to us, the fewer treatments we will have to be able to help you. Not only will the treatments potentially be less effective, but also they can be more dangerous. As you accumulate brain injury, then the risk for complications of the treatments increase as well. So time is brain in many different ways to think about it. You need to be seen immediately so you can be treated quickly before you have injury and with maximum amount of options for treatment that you can have.
What’s the most common type of stroke?
There are two types of strokes. The one where the vessels get clotted and blood is not getting through and the tissue beyond the vessels gets dry and dies. Imagine not watering your grass for a week. So the longer you wait to water the grass, the more grass you lose. In this case, in the brain, it takes five minutes for you to start losing your grass.
The other kind of stroke is where the vessels break and the blood gets out of the vessel and bleeds. We call that hemorrhagic strokes. In this case, you know, instead of not watering, you love the hose on outside and then your grass is full of water. That's exactly what happens to the brain.
The most common kind is the ischemic stroke, about 80%, and the hemorrhagic stroke is about 20%.
What should a patient or family expect when arriving at the ER?
Usually the EMS has called ahead, so there will be a lot of people waiting for the patient. We have processes in place to make sure everything happens very quickly.
The patient will get taken to a CT scanner quickly. We get the images quickly and we get through now artificial intelligence processes, we get to know very quickly which area of the brain is affected, how much and what kind of treatments we can offer.
They're going to be told about the options and usually given the odds of risks of the treatments. All these treatments have some risks, so we want when the patients are able to communicate and understand to be aware of those risks. When the patient cannot communicate, which unfortunately is quite often, then we use guidelines to help us make those decisions to treat them with the appropriate interventions. Those are either medications or taking them to the angio suite, where my colleagues and the vascular team will go from the inside of the vessels and fish the clots out of the brain to help them recover their functions.
Healthy Actions: New guidelines suggest heavy marijuana use be disclosed before surgery
How long does to take to recover from a stroke?
A stroke starts the day you have it, but it ends really at the end of your life. Your recovery from a stroke is a lifelong endeavor. It is important early on to engage in therapies, including speech, physical and occupational therapies. Sometimes patients need to learn how to walk again.
It's super important to have strong family support because it can be hard. This person may have been independent two days ago and is now dependent on everybody for everything. Sometimes you may need behavioral health assistance to help with depression that may come as a result of the stroke.
Healthy Actions is a look at a medical topic of interest with a local expert. To see previous columns, go to www.tinyurl.com/BettyHealthyActions
Beacon Journal staff reporter Betty Lin-Fisher can be reached at 330-996-3724 or blinfisher@thebeaconjournal.com.
Follow her @blinfisherABJ on Twitter or www.facebook.com/BettyLinFisherABJ To see her most recent stories and columns, go to www.tinyurl.com/bettylinfisher
This article originally appeared on Akron Beacon Journal: Healthy Actions: BE FAST to spot symptoms of a stroke

