What we learned from two hellacious years of COVID-19 at the county hospital for the poor
If you drive past Valleywise Health Medical Center in Phoenix, it’s hard to miss the construction site where a new hospital is emerging.
The 10-story tower – which will replace the aging hospital longtime residents know as “county” – represents a beacon of hope and renewal for the doctors, nurses and other clinicians who fought COVID-19 for the last two years.
It has been an exhausting and challenging time. Our health system disproportionately cares for people with low-incomes and communities of color, groups especially impacted by the pandemic.
In short, our hospital became a medical battle zone.
We had never seen so many severely ill patients
The children’s emergency department was converted into a COVID-19 intensive care unit, one of five in the hospital, and ER patients were triaged in the waiting room. At times, we felt overwhelmed. We had never seen so many severely ill patients, many struggling to catch their breath, and so much death.
Even today, the numbers seem unreal: Valleywise Health experienced 457 patient deaths due to COVID-19. We’ve treated and discharged 4,172 patients with COVID-19 and seen over 16,200 positive COVID-tests across our system.
Throughout the pandemic, we increased our ICU bed capacity by 33% and the number of adult beds by 20%. This led to demands for increased staffing across all disciplines and countless hours of overtime and extra work. Every single employee was impacted in one way or another.
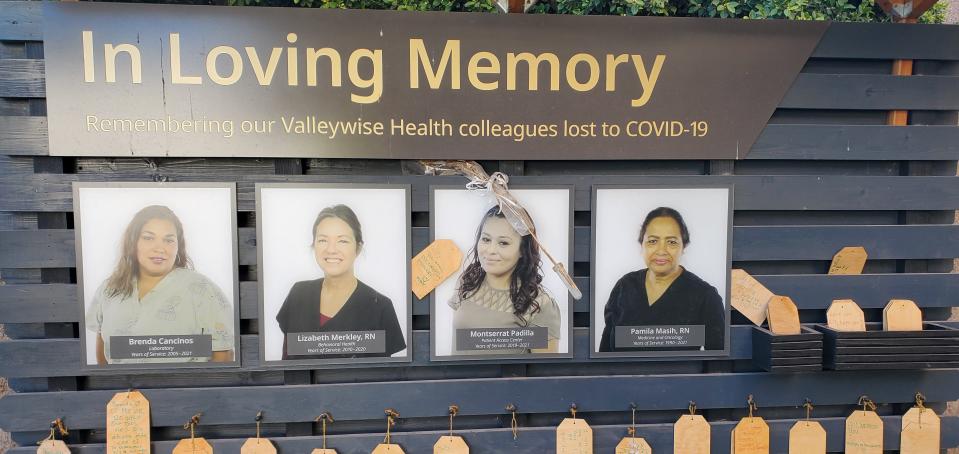
Our staff was not immune to the virus. Before a vaccine was available, four team members lost their lives to COVID-19. Their photos and names are posted outside the hospital in our healing garden. We will never forget them.
The pandemic represented one of the greatest threats our health care system has ever faced in its 145-year history.
Yet we held together, despite limited resources and a 52-year-old building. We relied on each other, boosted each other and rallied to deliver top quality care. We prayed, we cried, and we prayed some more.
Now, spaces are returning to their original functions
In 2020, we were thrilled when The Arizona Republic honored us and other health care workers as “Arizonans of the Year.” A year later, many of our patients and their families viewed us with skepticism and scorned our best medical advice. We learned to accept that we could not change their opinions.
Today, we have a handful of COVID-19 positive patients and have moved many spaces back to the original functions.
We are hopeful the virus will not come roaring back, but now we know we can handle just about anything. Yes, there is high health care professional turnover and burnout.
At the same time, there are fresh new faces on our floors, new nurses inspired by the pandemic and veteran staff who took to the road to work in communities with the most urgent needs during the pandemic are returning.
As new variants of the virus continue to emerge and fewer people opt to wear face masks, the profile of COVID-19 patients will continue to vary. Vaccines are still not available for children under 5, and many people still have chosen not to get vaccinated.
COVID-19 remains a threat and we need to remain vigilant and use the tools we have available to treat this illness, including vaccination and wearing a mask when transmission is high.
5 things we learned from COVID-19
We are better prepared because we have learned many lessons:
While doctors and nurses got the media attention, many others deserve the title of health care heroes. They include respiratory therapists who worked tirelessly to keep our patients alive and physical and occupational therapists who suited up in PPE to keep bed-ridden patients moving. The list goes on: speech therapists, pharmacists, interpreters, lab technicians, security, housekeeping staff and food service workers. Central sterile personnel tasked with prepping equipment came to work every single day to keep our hospital running, IT provided devices to help our isolate patients communicate with family members and facilities worked magic to turn our pediatrics emergency department into a COVID-19 unit.
Self-care is important. Throughout the pandemic, exhaustion and burnout became serious problems, especially when the Omicron variant hit in December 2021 and January 2022. The public provided amazing support through cards and food and equipment donations. Our leadership offered additional services, including counselors, meditation programs and emotional and financial support. It made a difference.
You can’t work in silos and be successful. When resources became hard to find, departments across our health care system had to collaborate and communicate better to serve our patients. We talked to each other more than ever before, and now we make better decisions than we did pre-pandemic.
Arizona hospitals are naturally competitive but work better together. Early in the pandemic, a group of hospital chief medical officers came together with the Arizona Department of Health Services and developed a statewide surge line to ensure a flood of COVID-19 patients during our peaks could get the care they needed and deserved. Nursing leaders shared best practices through statewide forums established by the Arizona Hospital and Healthcare Association. These initiatives prevented hospitals – and staff – from being overwhelmed.
We could not do this important work without public support. We are extremely grateful to taxpayers who support the historic mission of Valleywise Health and those who support us through the Valleywise Health Foundation. Thanks to Maricopa County voters, who overwhelmingly passed our bond election in 2014, Valleywise Health is building a new hospital, scheduled to open October 2023, and new health clinics across the Valley.
We learned to be tough, and hug each other a lot
Valleywise Health Medical Center, at 24th and Roosevelt streets, opened in 1971 as Maricopa County General Hospital and was renamed Maricopa Medical Center in the 1980s by administrators trying to shed the “county” image.
We’re no longer part of Maricopa County (voters approved a special health care district in 2003), but many of us still proudly wear the “county” moniker. It denotes a toughness, an ability to do more with less and a pride that we take in caring for the neediest.
During the pandemic, that esprit de corps was more evident than ever. Nurses reassured and hugged each other in the darkest times, our medical residents stepped in to staff our COVID-19 units and physicians worked endless hours.
Every day, we’re inspired by co-workers who provide kind, compassionate care to each patient, every time. Working here is truly a calling; we wouldn’t have it any other way.
Dr. Mark MacElwee, District Medical Group, is an internal medicine specialist at Valleywise Health Medical Center. Jennifer Granger, BSN RN, is a nurse manager at the medical center. Reach them at Mark_MacElwee@dmgaz.org and jennifer.granger@valleywisehealth.org.
This article originally appeared on Arizona Republic: What 2 years of COVID-19 hell taught our county hospital

