Leprosy could now be endemic to Central Florida, researchers say. Here’s what to know
Leprosy, an easily curable disease that affects the skin and nervous system, may already be endemic to Central Florida — where it’s suspected to now have a constant presence, according to a report released in a U.S. Centers for Disease Control and Prevention journal.
The illness, also called Hansen’s disease, can result in paralysis of the hands and feet and blindness if left untreated. Unlike COVID-19, prolonged and close contact with someone with untreated leprosy over many months is needed to catch the disease, and the vast majority of people are not susceptible to infection with the bacteria that causes it, health officials say.
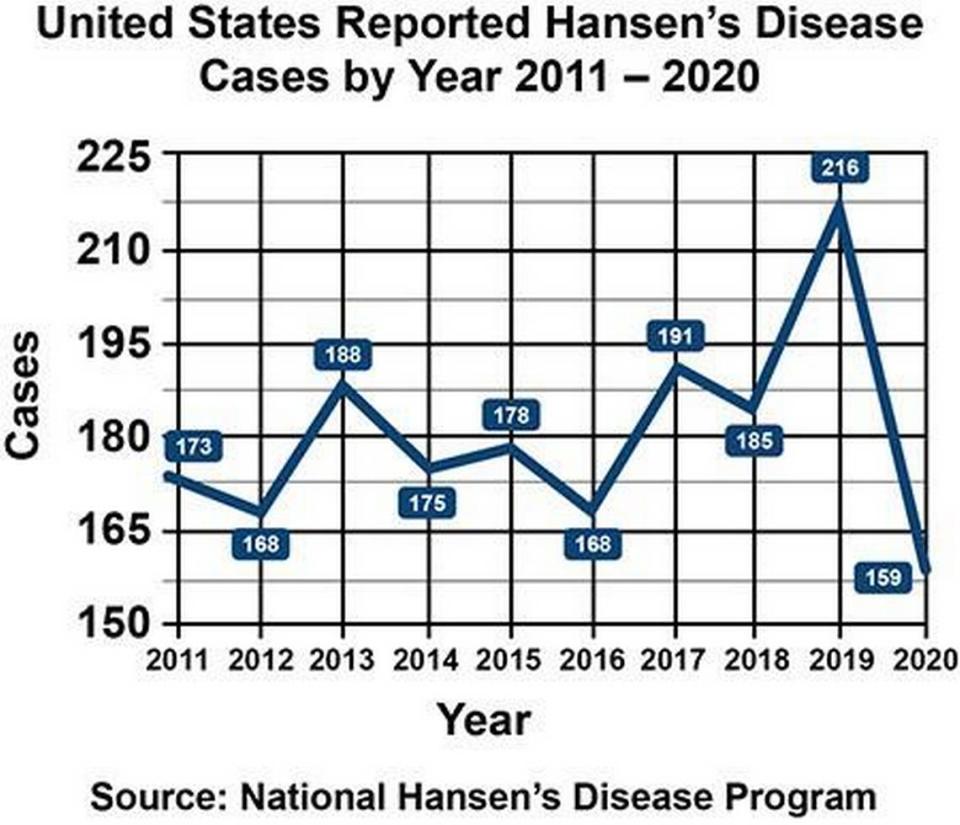
Instances of leprosy are spiking in Florida, where 16 cases have been confirmed so far this year, 11 more than during the same time period last year, data from the state’s health department shows. About 150 to 250 leprosy cases in the U.S. are reported each year, the CDC says, and Florida is among the states at the top of the list.
An increase of cases lacking traditional risk factors, such as traveling outside of the United States, suggest that the disease is endemic to Central Florida, the researchers noted in a report published in the August edition of the CDC’s Emerging Infectious Diseases journal. When a disease becomes endemic, it means that it is regularly occurring in a particular region.
An endemic disease differs from a pandemic because the cases are somewhat contained and not spreading out of control. When a disease is endemic, actions can be taken to prevent it from spreading and from causing significant disruption in our daily lives.
“Those trends, in addition to decreasing diagnoses in foreign-born persons, contribute to rising evidence that leprosy has become endemic in the southeastern United States,” the researchers said.
Why is this important?
Leprosy incidents peaked around 1983 in the U.S., and a drastic reduction in the annual number of documented cases occurred from the 1980s through 2000. But the number of reported cases has more than doubled in the southeastern U.S. over the last decade, the researchers say.
Of the 159 new cases reported in the U.S. in 2020, the most recent year for which data is available, 110 or 69% of them were reported in Florida, California, Louisiana, Hawaii, New York and Texas, according to the National Hansen’s Disease Program, a service of the U.S. Department of Health and Human Services primarily responsible for inpatient and outpatient care and treatment of people with the illness.
Central Florida accounted for 81% of cases reported in Florida and almost one fifth of nationally reported cases in 2020, the researchers said. The Florida counties with the most cases from Jan. 1 to July 31 are Brevard with four and Volusia with three, according to data from the Florida Department of Health. The counties of Bay, Bradford, Charlotte, Flagler, Highlands, Palm Beach, Pinellas, Polk and Seminole have reported one case each.
Several cases in the region, the report’s authors noted, demonstrate no clear evidence of traditionally known risk factors: traveling, infections that are spread between people and animals and personal contact with people who have the disease.
A recent systematic review of studies conducted during 1945–2019 supports an increasing role of transmission of the disease from human to animals and from animals to humans but many cases reported in eastern United States, including Georgia and Central Florida, didn’t involve animals or traveling outside of the U.S, the researchers said.
Given those studies, and the researcher’s analysis of a 2022 leprosy case in Central Florida, they noted there is “some support” for the theory that international migration of persons with the disease is a potential source of transmission between person to person in the same place.
“Our case adds to the growing body of literature suggesting that central Florida represents an endemic location for leprosy,” the researchers said. “By increasing local physician efforts to report incidence and supporting further research to assess routes of transmission, a congruent effort can be made to identify and reduce spread of the disease.”
But leprosy remains a very uncommon illness in the U.S., Dr. Charles Dunn, one of the report’s authors and chief dermatology resident of the Kansas City University-GME Consortium / ADCS program in Orlando, told the Miami Herald.
“We do not want to be spreading fear. That was not the purpose of the article, nor do we think that leprosy is a problem that is rampant in the United States,” Dunn said in an email Tuesday night. “Our paper simply highlights that there appears to be an intriguingly strong geographic predilection for leprosy in Central Florida.”
The CDC hasn’t declared leprosy endemic to Central Florida, and no related travel advisories have been announced. The Florida Department of Health didn’t immediately respond to an emailed request for comment sent Tuesday afternoon.
What is leprosy?
Leprosy, renamed after the Norwegian scientist Gerhard Henrik Armauer Hansen who discovered it in the 19th century, is an infection caused by a bacteria called Mycobacterium leprae, which can grow very slowly and it may take up to 20 years to develop signs of the infection, according to the CDC.
In the past, the disease was feared as a highly contagious, devastating disease, but now scientists know that it’s hard to spread and it’s easily curable after it’s detected with a course of antibiotics.
Are there symptoms?
The disease can affect the nerves, skin, eyes and lining of the nose, the CDC says, by attacking the nerves and causing inflammation under the skin. This can cause the affected areas to lose the ability to sense touch and pain, which can lead to injuries, like cuts and burns. Usually, the affected skin changes color and either becomes:
▪ lighter or darker, often dry or flaky, with loss of feeling, or
▪ reddish due to inflammation of the skin.
How does leprosy spread?
It’s not known exactly how the disease spreads between people, the CDC says, but scientists currently think it may happen when an untreated person with the disease coughs or sneezes, and a healthy person breathes in the droplets containing the bacteria.
Unlike COVID-19, prolonged and close contact with someone with untreated leprosy over many months is needed to catch the disease, according to the CDC. People can’t get leprosy from casual contact with a person who has the disease like shaking hands, hugs and sitting next to each other.
“There does appear to be an association with 9-banded armadillos so caution should be exercised by the public when direct contact with these animals,” Dunn said.
According to the National Hansen’s Disease Program, around 95% of people are not susceptible to infection with the bacteria that causes leprosy.
Can leprosy be treated?
Leprosy can be easily treated, according to the CDC.
Early diagnosis and treatment with three antibiotics usually prevents disability that can result from the disease, and people with the disease can continue to work and lead an active life.
Once treatment is started, the person is no longer contagious, but it’s essential that the patient finishes the entire course of treatment, which may last one to two years, as directed by their doctor.

