How losing TennCare due to mail mix-up impacted a Tennessee mother
More than 112,000 Tennesseans dropped so far from TennCare health coverage during a massive audit of statewide eligibility lost benefits because of paperwork issues.
Including 1-year-old Emma Lyngar, who suffers from congenital vocal cord paralysis.
Several months ago, her mother, Hannah, changed her address. State forms never reached their new home in Clarksville.
Hannah Lyngar discovered the issue when Emma's routine hospital checkup, which included tests, ended with out-of-pocket bills totaling $259. While TennCare eventually re-enrolled Emma, her mother was stuck with medical bills from the coverage gap.
"So, it's a big hit for me," Lyngar said.

Recently divorced, Lyngar's monthly take-home pay for loading tires on trucks is about $2,100. Her family funds shrink drastically after paying rent ($1,795). Hannah's five siblings moved in on Oct. 13.
"There's no wiggle room at all. I'm just trying to figure out how to feed six kids."
TennCare's yearlong audit of beneficiary eligibility is entering its fourth month. TennCare officials have predicted that 350,000 Tennesseans could ultimately lose coverage — largely because they are no longer financially eligible.
Losing TennCare eligibility: How did this happen?
According to recently released TennCare data, 59% of beneficiaries have been either auto-renewed for benefits or responded to state checks and were determined to be eligible. Some 35,000 have been found to be ineligible; they were referred to the individual insurance marketplace (sometimes referred to as "Obamacare") at Healthcare.gov.
Yet 112,178 more, state records show, either failed to respond, failed to respond to state inquiries or did not provide all of the requested information to confirm continued TennCare eligibility. They represent about 76% of the rejected total, a figure that upsets Michele Johnson, the executive director of the Tennessee Justice Center, a nonprofit advocacy group.
"There's a process that's supposed to be set up that people can navigate," Johnson said. "Seventy-six percent of those who have been terminated have been terminated because of a procedural reason — meaning they don't know whether they're eligible or not, which is really damning.
"People are losing coverage who desperately need that coverage."
The Tennessee Justice Center is suing the state over the way it determines who is eligible. A trial in that case is scheduled to start next month.
Related coverage: Why has TennCare dropped 57K Tennesseans after eligibility reviews?
More: At least 220,000 Tennessee kids faced loss of health insurance due to lacking paperwork
Health care disenrollment nationwide vs. Tennessee
Tennessee is not alone in accumulating such a high percentage of procedural disenrollments, according to information collected by KFF, a health policy research organization. If anything, Tennessee's 76% rate is roughly in the middle of the pack.
Some states tally rates above 90%.
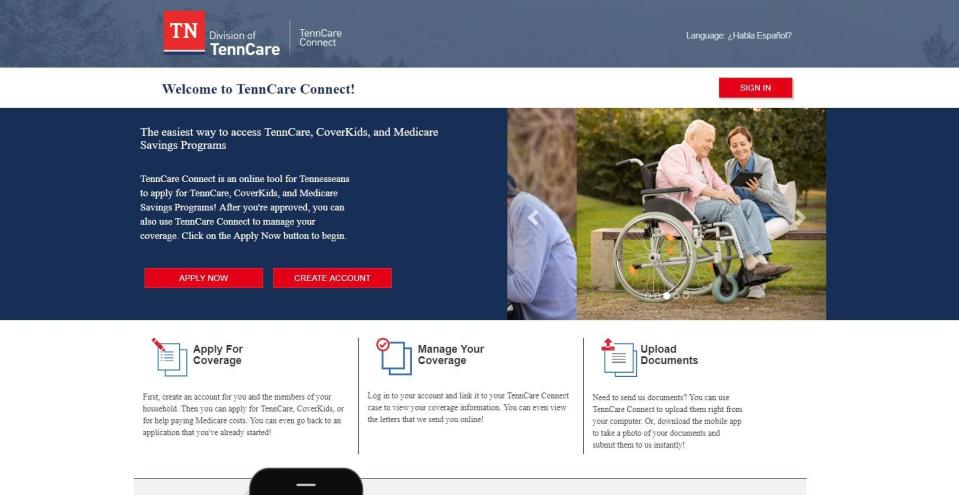
How do I check my TennCare status?
TennCare has urged beneficiaries to contact the agency online to confirm their contact information, and/or keep an eye out for mail from the agency. The online portal is at tenncareconnect.tn.gov. Beneficiaries may also call 855-259-0701.
Johnson argues that many Tennesseans don't have access to reliable internet and/or may move or disregard what might otherwise look like junk mail. She added that residents who receive TennCare forms are often confused by them.
A better solution, she argued, is to expand Medicaid eligibility in Tennessee — an option the state's Republican leadership has steadfastly opposed.
TennCare enrollment status: 'No way of knowing for certain until we complete the process'
TennCare enrollment as of September was just over 1.7 million, according to the state. Enrollment in March 2020 was about 1.4 million.
"Our best projection is that we will return to pre-pandemic enrollment once we’ve completed the unwinding; however, we will also continue to add new members during that time," TennCare spokeswoman Amy Lawrence said in an email. "This is just an estimate and we have no way of knowing for certain until we complete the process and determine eligibility."
Beneficiaries who lose coverage during this process are granted a 90-day reconsideration period to update their information with the state, Lawrence noted.
Though, as in the case of the Lyngars, that wait time can lead to unexpected, out-of-pocket costs.
Editor's note: This story has been updated to state the correct date when Emma Lyngar's five siblings moved in with her and her mother.
Frank Gluck is the health care reporter for The Tennessean. He can be reached at fgluck@tennessean.com. Follow him on X at @FrankGluck.
Want to read more stories like this? A subscription to one of our Tennessee publications gets you unlimited access to all the latest political news, plus newsletters, a personalized mobile experience, and the ability to tap into stories, photos and videos from throughout the USA TODAY Network's daily sites.
This article originally appeared on Nashville Tennessean: TennCare drops about 150,000 in Tennessee amid beneficiary audit
