Measles, mpox, Marburg virus, oh my! Here's why we're seeing so many emerging infections

Before the appearance of COVID-19, most parents may not have thought much about pandemics and their effects on our personal and public health. But consider this: Even as society learns to live with this new coronavirus, other infections have been creeping into the headlines, including measles, mpox (previously called monkeypox) and Marburg virus disease.
Medical providers and the community alike are asking: "Are we seeing more emerging infections? And what can we do to stop future outbreaks?"
Lessons from the COVID-19 pandemic can be applied to other infectious threats:
Stay home from work, school, or daycare when sick. A mild respiratory infection for you or your child, even if not COVID-19, can be a life-threatening illness for someone else.
Keep vaccines up to date. Vaccination is a cornerstone for preventing infectious outbreaks.
Consider participating in a vaccine trial to help advance the science.
In higher-risk settings like a medical waiting room or an airplane, wear a face mask − especially during surges of different infections.
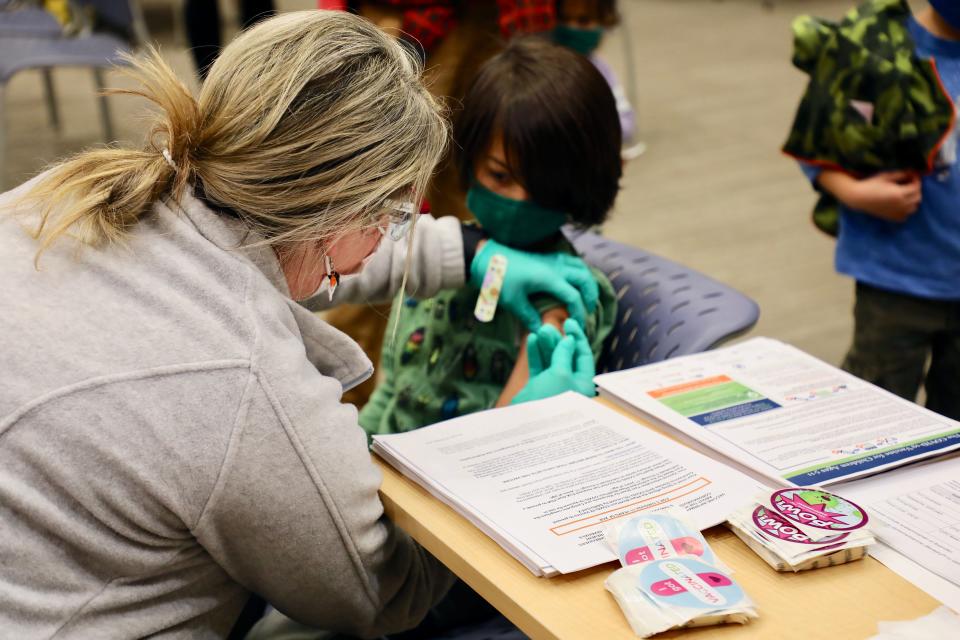
What is contributing to these infectious outbreaks? Early in the pandemic, many families were unable to easily access preventive medical care. Childhood vaccines essential to preventing outbreaks were delayed by some families. And with rampant misinformation online about vaccine safety and efficacy, others became hesitant to proceed with previously well-accepted immunizations.
For example, measles vaccination rates in Ohio kindergartners dropped from 96.2% in 2014 to 89.6% in 2021, which is below the 95% uptake required for herd immunity and prevention of outbreaks. This has been reflected by three unrelated measles clusters in unvaccinated individuals in the Akron and Columbus areas of Ohio as well as Jessamine County in Kentucky over the past year. Dozens of children got so sick they had to be hospitalized − with an infection that can be prevented with a vaccine!
The good news is technological advances amid the COVID-19 pandemic led to improvement in identification and monitoring of outbreaks. For example, scientists have implemented wastewater monitoring for severe acute respiratory syndrome coronavirus 2, which gives us an early signal for when we might see surges in COVID-19 infections. Enhanced surveillance will result in more reports of outbreaks like polio detected in New York waterways in 2022. Early detection can identify and stop outbreaks before they become widespread.
The pandemic emergency is over. What does that mean for hands and elbows, vaccines, more?
As the world population grows, humans and nature interact more − and that provides opportunities for pathogens to jump from animals to people and cause new infections. Deforestation forces animals into urban settings.
Urbanization can overcrowd neighborhoods, and as a result viruses and bacteria spread more easily. The Ebola virus outbreak in West Africa in 2014-16 was likely widespread because people lived in cities with poor sanitation, which amplified transmission.
Continued expansion of air travel brings new infections to other parts of the world in a few hours. The mpox outbreak of 2022 spread to 110 countries within weeks as travelers to endemic regions brought the virus home.
Temperature instability from climate change allows pathogens to spread geographically. Lyme disease, a tickborne infection, used to be rare in southern Ohio but has been rising since the 1990s as fewer ticks die during our increasingly warm winters.
While infectious outbreaks are occurring more frequently based on factors such as climate change, decreased vaccination rates, and globalization, how much that impacts Cincinnatians will be variable.
Experts suggest we will experience other emerging or reemerging infections in our community during our lifetimes, but those might not be as largescale as the COVID-19 pandemic.
As parents, we can protect our families by keeping kids home when sick, ensuring they get vaccinated, and reminding them to wash their hands.
Dr. Felicia Scaggs Huang, a pediatrician, is Cincinnati Children’s director for Infection Prevention & Control.

This article originally appeared on Cincinnati Enquirer: Drop in vaccinations related to more infectious outbreaks | Opinion

