Medicaid eligibility verification drops 32,000, including 16,000 kids, from benefits
For the first time in three years, Medicaid enrollees are having their eligibility for benefits verified, finding more than 32,000 people ineligible for health care coverage in June.
About half of those now without health care coverage are children. Many of the people who lost coverage were disenrolled for procedural reasons, meaning that some portion of their eligibility documentation is missing.
About 116,000 people had their eligibility checked in June by the Department of Social Services. This resulted in about 43% keeping coverage, 28% deemed ineligible and 29% with pending coverage determinations.
“Of course, it's very frustrating, but I'll be honest with you, that it's not very surprising.” said Crystal Quade, the Missouri House Minority Leader and 2024 gubernatorial candidate.
This is the first of 12 verification periods for roughly 1.5 million Medicaid recipients. With Missouri’s population coming in at over 6.1 million, that means about a quarter of the state was enrolled in Medicaid.
During the pandemic, federal law prohibited states from revoking health care benefits, but annual eligibility verification was a common practice prior to 2020.
However, since Medicaid expansion was implemented in 2021, which expanded eligibility to some adults, many of the enrollees have never experienced the verification process. This raises concerns that some may not know they need to verify their eligibility.
“I've had many families reach out to me and say, ‘I didn't realize I had to send records back in. It just said I was kicked off,’” Quade said. “It’s not very clear what the situation is when these families receive notices.”
The state has engaged in a number of outreach campaigns apart from the direct notices from DSS to notify Medicaid recipients of the need to verify their eligibility.
“We have a number of public awareness campaigns going on through social media, radio, and traditional media, as well as working with providers and partners around the state like doctors and hospitals and pharmacies,” said Caitlin Whaley, spokesperson for the Department of Social Services.
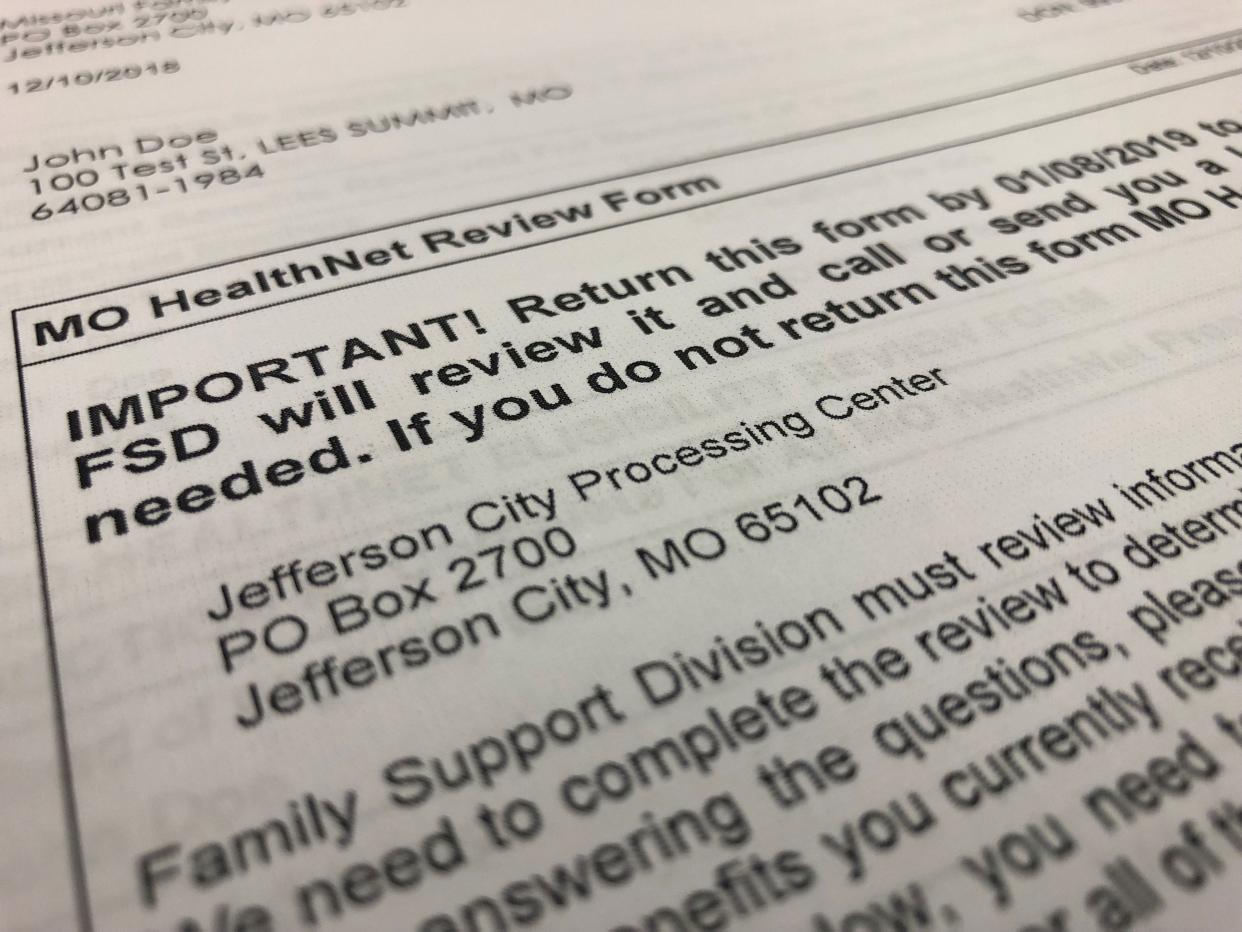
Those currently receiving Medicaid benefits will receive notice that their eligibility will be renewed about a month before their renewal date. Information must be provided by the deadline, either by phone at 1-855-373-4636, digital upload at myDSSupload.mo.gov or in-person at a local resource center, listed at myDSS.mo.gov/renew.
Those that lost healthcare coverage have a variety of options for obtaining it again, though it depends on the situation.
For those losing coverage for procedural reasons, DSS offers a 90-day period in which recipients can verify their eligibility by providing the missing documentation. The agency already sent notices to any recipients lacking the proper paperwork that include forms to complete their eligibility profile.
“All they have to do is fill it out and send it back, and the agency will turn their eligibility back on and there will be no lapse in their coverage,” Whaley said.
More: If you're one of 1.4M Missourians on Medicaid, confirm your contact info before April 1
Some enrollees had their coverage canceled because they were found ineligible due to their income or other factors. Some of these people were already recommended to enroll in coverage through the Health Insurance Marketplace created through the Affordable Care Act on HealthCare.gov.
“There are mechanisms in place for people that get disenrolled to connect them to the ACA marketplace,” said Sheldon Weisgrau, the Missouri Foundation for Health’s vice president of health policy and advocacy. “So all that is helpful, but nevertheless, we just don't have a healthcare system in place that prevents people from dropping through the cracks.”
Others are advised to visit Cover Missouri’s website, which is a project aimed at securing health insurance for Missourians from the Missouri Foundation for Health. They should also speak with their employer about potential health care benefits through their job.
However, many people who have received Medicaid benefits find that their eligibility is always in flux for reasons related to their income or employment status. This process is known as churn, which involves people teetering between being eligible and ineligible for Medicaid.
“That process is very disruptive to people's ability to get consistent health care services.” Weisgrau said. “So we just don't have a really seamless system in this state or in this country to make sure people stay enrolled.”
This article originally appeared on Springfield News-Leader: Medicaid eligibility verification drops 32,000 people from benefits

