Modernizing rural healthcare: West Texas medical experts say technology, reforms needed to boost rural health
The effects of the COVID-19 pandemic can still be felt today in the healthcare system; however, West Texas medical experts say there is an urgent need to modernize the system to better accommodate rural communities.
Even though larger institutions are stepping up to help rural communities, their leaders agree that there are some obstacles preventing them from serving the rural communities more effectively.
Broadband access
A common issue mentioned by leaders with the Texas Tech Health Sciences Center HSC and Covenant Health is connecting rural areas to broadband infrastructure for telehealth.
“During COVID, when everything was going online - from education to healthcare - one of the things that we immediately saw was that our healthcare can only go as far as our broadband,” TTUHSC President Lori Rice-Spearman said. “We still had communities out there that were not being served.”

Rice-Spearman said the institution is now moving into a “technology-based healthcare ecosystem” in the future.
“We're making sure we have the infrastructure in place to support not just our university but the communities around us,” she said. “So how do we work with those communities to make sure that they have the technology in place so that the gap doesn't widen? The last thing we want is for the rest of the world or the rest of Texas to be moving towards this high-tech type of healthcare and that the rural communities get left behind.”
During the pandemic, Rice-Spearman said, the university got creative in providing broadband access to the communities.
“We were able to do some very innovative and creative things like buses and telehealth and putting things in parking lots so that they could come and get access to telehealth and healthcare that way,” she said.
Walter Cathey, regional CEO of Covenant Health System, said the telehealth system isn’t viable to sustain itself at this point.
“It’s still way too costly, and we can't get to scale,” he said. “That's really the big push on that is to figure out how to drive the cost down of telehealth to where these rural places can afford it.”
On average, a rural hospital will make a profit of $40,000 to $50,000 per year and telehealth equipment costs over $100,000, Cathey said.
Covenant is looking into using the foundation's money to create a subsidized model to create a way to curve the cost of the equipment for rural hospitals, he said, in the upcoming two years.
The Texas Legislature also took up this issue in its last session and passed House Bill 5.
According to an opinion column submitted but Glenn Hegar, Texas State Comptroller, HB 5 was an answer to a problem that was arising due to 4.5 million Texans using telehealth medicine during the pandemic.
The bill allocated $5 million to create the Broadband Development Office to implement legislation on broadband expansion.
The state received more than $500 million from the American Rescue Plan Act to help with broadband expansion, and an additional $100 million from the Infrastructure Investment and Jobs Act.
However, there are more challenges rural health needs to overcome.
Laws and regulations
National laws are also preventing rural communities from receiving critical funding to keep rural healthcare alive.
Cathey said there is a distinction that rural hospitals can receive known as a critical care hospitals. This allows the federal government to cover all expenditures the hospital makes.
However, some local rural hospitals are not receiving this distinction due to a technicality.

“The rule is you need to be 35 miles from the closest approximate hospital to be licensed as a critical access hospital,” he said. “If you look at the geography of West Texas, they're these perfect little boxes, right? And pretty much every hospital sits at the county seat. They're exactly 30 miles apart from each other.”
Since they are five miles too close to each other, rural hospitals are missing out on receiving critical funding that could help bolster their services to the community it’s serving.
It also means the hospitals are struggling financially to keep open their doors.
Cathey said Covenant is facing this issue because Covenant’s Levelland hospital is five miles too close to Lubbock’s hospital.
“We lose a couple of million dollars a year just on Levelland to keep that hospital going, but it's the right thing to do for the community,” he said. “We wouldn't lose that money if it was designated as a critical access hospital and neither would any of the other ones in West Texas but it's an old rule — it's not built on our geography and it hinders us.”
The Lubbock Avalanche-Journal complied data from the Texas Agriculture Commissioner's website and the Texas Health & Human Services website and found that there are 14 critical access hospitals in the local area and six rural hospitals.
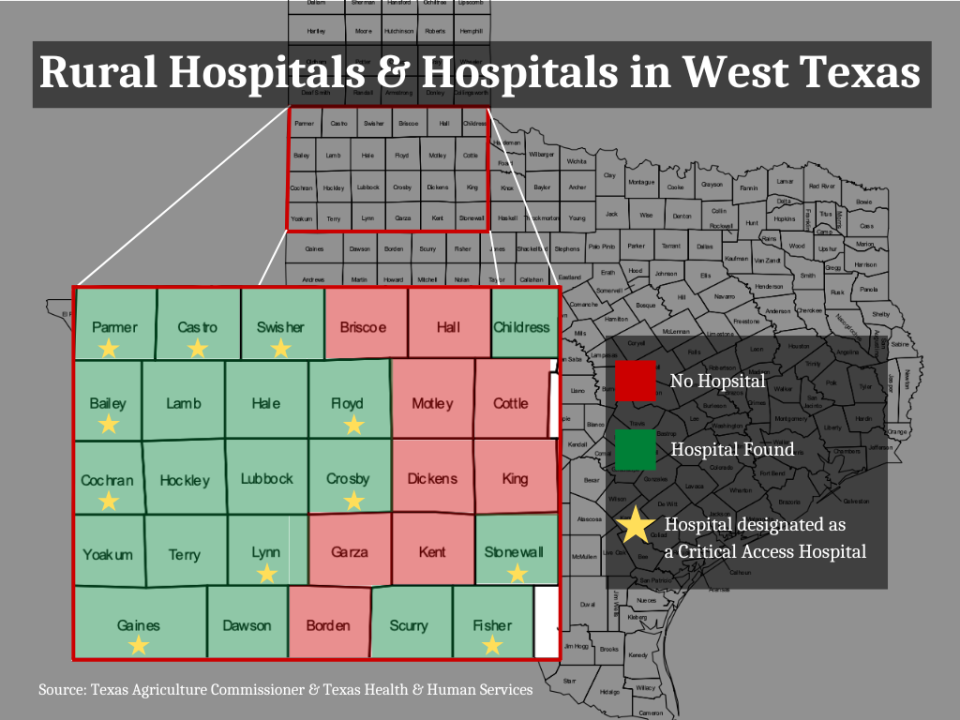
The list contains all 29 counties that were looked at, if the county has a hospital(s) and if it has a CAH designation:
Parmer- yes, CAH designation
Castro- yes, CAH designation
Swisher- yes, CAH designation
Briscoe- no hospital found
Hall- no hospital found
Childress- yes, no CAH designation
Bailey- yes, CAH designation
Lamb- yes, no CAH designation
Hale- yes, no CAH designation
Floyd- yes, CAH designation
Motley- no hospital found
Cottle- no hospital found
Cochran- yes, CAH designation
Hockley- yes, no CAH designation
Lubbock- yes, no CAH designation
Crosby- yes, CAH designation
Dickens- no hospital found
King- no hospital found
Yoakum- yes, CAH designation
Terry- yes, no CAH designation
Lynn- yes, CAH designation
Garza- no hospital found
Kent- no hospital found
Stonewall- yes, CAH designation
Gaines- yes, CAH designation
Dawson- yes, no CAH designation
Borden- no hospital found
Scurry- yes, no CAH designation
Fisher- yes, CAH designation
With nine out of the 29 counties having no hospital, 14 counties having a CAH hospital and seven counties having regular hospitals, and the constant financial uncertainty, the need to grow and support rural health care is there.
This article originally appeared on Lubbock Avalanche-Journal: Growing need to modernize healthcare to better serve rural communities

