'Never expected this to happen in the US': How the COVID-19 pandemic exploded from March to December
As the COVID-19 pandemic rages unabated across the United States, December is already breaking records – only a week in.
Public health experts warned for some time that a winter surge would come. But four who spoke with USA TODAY said they have been stunned by the dismal trajectory of the virus over nine grueling months, and they never expected the nation to be in as bad a position as it is right now.
"I don't think there's a single person anywhere who thought that we would still be facing this in December, let alone that this would be at such a peak at this particular time," said Dr. Robert Amler, dean of New York Medical College's School of Health Sciences and Practice and a former chief medical officer at the federal Centers for Disease Control and Prevention.
Ali Mokdad, chief strategy officer for population health at the University of Washington, is more blunt: "I never expected this to happen in the U.S."
As the nation slides into a dark and dangerous winter and states are turning to stricter restrictions and lockdowns, what has changed since March and how did it go so wrong?
Stark numbers of deaths, hospitalizations tell the story
On March 31, a White House prediction said 100,000 to 240,000 could die by the end of the year. More than 2 million would die without social distancing and other mitigation. The latest modeling, however, from the University of Washington's Institute for Health Metrics and Evaluation projects more than 345,000 deaths by Jan. 1.
Monica Schoch-Spana, a senior scientist in the Department of Environmental Health and Engineering at the Johns Hopkins Bloomberg School of Public Health, called COVID-19 in the U.S. "a protracted, open-ended and ongoing type of crisis."
"I assumed this would have gotten under control like it did in other countries," she said. "I didn't expect that we would have such a fragmented and uneven response that would keep us in such an acute stage of the crisis."
Coronavirus surge: How a third wave of COVID-19 engulfed the US
The U.S. saw its two deadliest days last week, surpassing the daily death peaks of April, according to Johns Hopkins data, as Wednesday reached 2,804 deaths and Thursday reached 2,879 deaths.
Friday, with 2,607 deaths, had the same number of fatalities as what had been the the country's worst day since the start of the pandemic, April 15.
"Where we are right now, in my personal opinion, is it's not unexpected but it's higher than we thought it would be," said Jennifer Balkus, an infectious disease epidemiologist at the University of Washington School of Public Health.
Before December, there hadn't been more than 2,500 deaths in a single day since April 29, when 2,527 people died.
Only eight days since the start of the pandemic have seen more than 2,500 deaths in the U.S. Four were in April. Four are in December.
"We are in a bad position," said Mokdad, also a professor at the health metrics institute.
COVID-19 hospitalizations near 100,000 in US. And experts fear facilities soon be 'overrun' by patients and a lack of staff
Hospitalizations across the U.S. have soared past where they peaked in April and later in July.
Hospitalizations in April and July never surpassed 60,000 people on a given day, according to the COVID Tracking Project's data, but in this surge of the virus, hospitalizations have mounted. The U.S. moved past the 60,000 threshold on Nov. 10 and has increased almost every day since, passing the 100,000 mark on Wednesday.
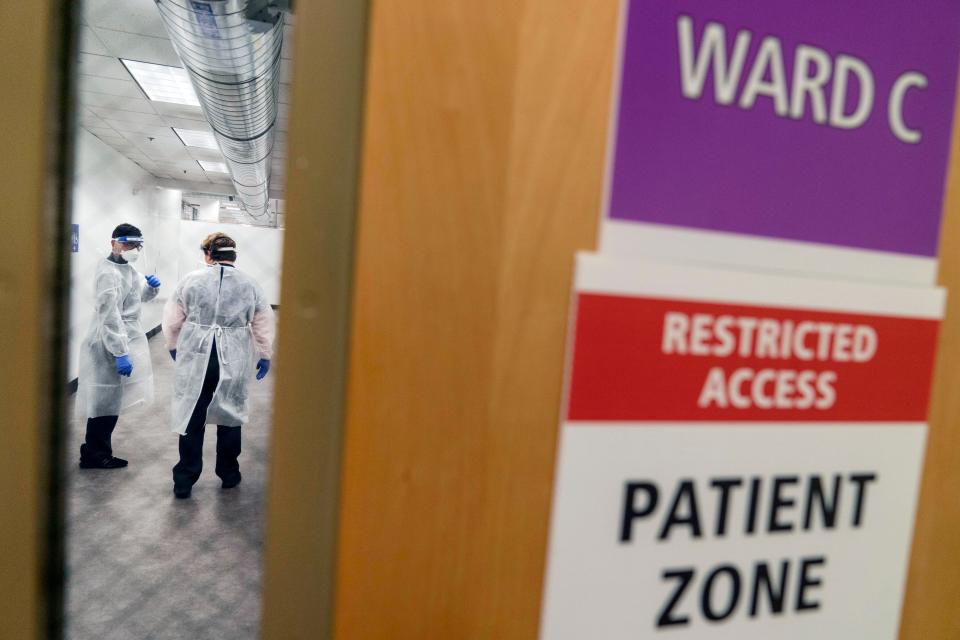
Balkus said she's worried because peaks in hospitalizations precede peaks in deaths, meaning even more records will be broken. "Given where we are right now, it's really concerning," she said.
A summer respite that never happened
Some epidemiologists thought the worst of the virus was happening in April, Mokdad said. The hope, he said, was to get cases to a more manageable level in the summer months. Then, when the weather turned cold and people spent more time inside, community spread would be at a level where testing and contact tracing could be effective.
That didn't happen. Instead many states prematurely reopened and the U.S. saw summer peaks, Mokdad said.
Schoch-Spana said the U.S. had the tools in place for a better pandemic response. "Had they been applied I think we would have had a different outcome, regardless of what we did or did not know about the virus itself."
For Schoch-Spana, the politicization around the virus and the U.S. response is an area where there has been consistency – but to the country's detriment.
The racial scapegoating of China, the lack of national support for mask wearing and the rush to promote drugs such as hydroxychloroquine were all tactics to manipulate public perceptions of the pandemic for political reasons, she said.
"The Trump administration saw value in social fragmentation. And that's the one thing you can't have in the middle of a pandemic," she said. "It has prevented the country and localities from pulling together in the same direction."
Amler said one of the biggest changes from March through December has been scientists' understanding of the role of airborne transmission and asymptomatic infections.
That shift in understanding of transmission highlights how important the changed guidance on masks was, Balkus added, saying she wished the U.S. overall had done better early on in trying to understand that the nature of the pandemic was evolving.
What we know about face masks has changed: Here's what experts say and which states mandate masks
"Changes in guidance are not a bad thing when you're trying to understand the dynamics of a brand-new virus," she said. "Updating guidance, that's good ... (and) one of the areas where we could have done better."
Some strategy hasn't changed
While doctors and public health officials have a greater respect for how the virus is able to spread compared with the early days, Amler said, the guidance of avoiding others to block exposure has not changed.
"The overall strategy is if there's no exposure, there can be no infection, and if there is no infection, there's no illness, and if there's no illness, there's no risk," he said.
Social distancing: It’s not about you, it’s about us
"I think that's one of the challenges," Balkus said. "The tools we have had since April are the tools we have now. That consistency is good, but it can feel frustrating.
"We are in that same place of being socially distant, washing your hands and wearing a mask."
According to a Gallup poll at the end of October, 62% of Americans said that their lives were "not yet back to normal."
But some may be less likely than in April to stay home if new stay-at-home orders were introduced, such as in California.
In the same Gallup poll from Oct. 19 to Nov. 1, just under half of Americans said they would be "very likely" to stay home for a month if public health officials recommended doing so because of a serious outbreak in their communities.
A Gallup poll from March 30 to April 5, however, showed that 67% of people said they'd be "very likely" to stay home.
California reintroduced stay-at-home orders for most of its residents this week, and many other states are reinstituting similar restrictions on bars, restaurants and other businesses that had been enacted in the spring and rolled back over the summer and fall.
Data shows some people have returned to traveling, too.
The Transportation Security Administration saw its busiest day of fliers since March on Nov. 29 as more than 1.1 million people passed through its checkpoints.
Holiday travel: CDC says Americans should avoid travel during winter holiday season, get COVID-19 tests if they do
Before that day, more than 1.1 million people hadn't passed through TSA checkpoints since March 16.
While much of the travel could be attributed to the Thanksgiving holiday, TSA numbers from throughout October and November indicate many people are flying again. The U.S. crossed the 1 million screenings in a day threshold for the first time since March on Oct. 18, and numbers never dipped below 560,000 in either month. The low in April bottomed out to as few as 87,534 fliers screened on the 14th.
Cellphone mobility data tracked by the Institute for Health Metrics and Evaluation also shows less social distancing. Though mobility has leveled off in recent weeks, the change is still much higher than the declines seen at the end of March and early April.
Better treatments and now the 'home stretch'
Unlike in March and April, how doctors treat COVID-19 is a positive change in the fight against the pandemic, Mokdad said.
The U.S. Food and Drug Administration has eight active emergency use authorizations for drug and biological products to treat COVID-19. One drug, remdesivir, has received approval for treating COVID-19 in adults and children 12 and older and weighing at least 88 pounds.
Among the options available to doctors treating COVID-19 patients are antibody, convalescent plasma and antiviral therapies.
Mokdad said such treatments have led to a decrease in hospital fatality rates. Overall case fatality rates have dropped over the course of the pandemic in the U.S.
"Clinicians have learned, sadly the hard way, how to better manage" COVID-19, Schoch-Spana said.
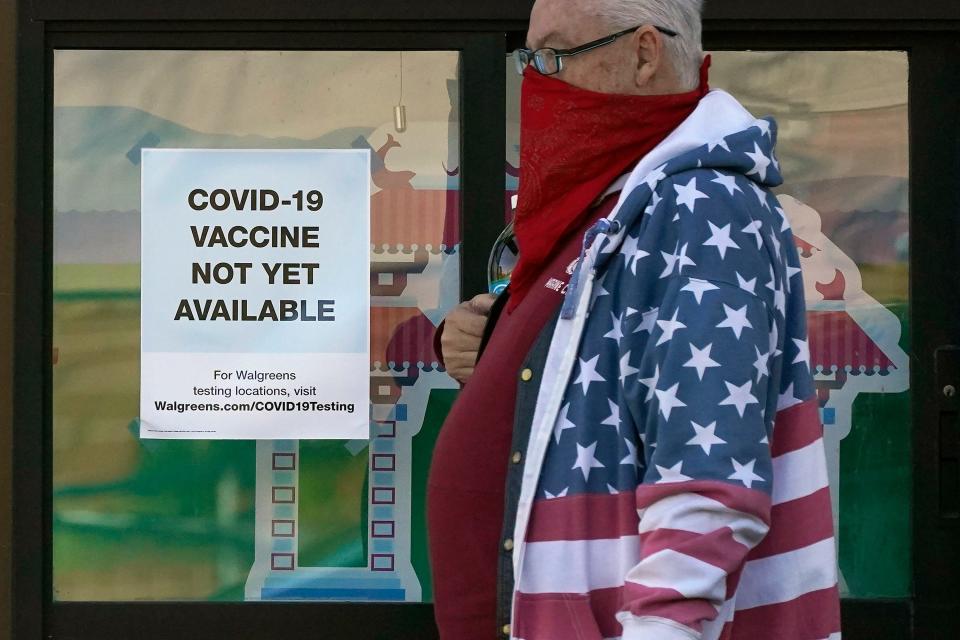
COVID-19 vaccine: Side effects from the COVID-19 vaccine means 'your body responded the way it's supposed to,' experts say
The nation also is closer than ever to having a vaccine authorized for use. "Although we are not at the finish line, I think we're beginning to get into a home stretch," Amler said.

The FDA could grant emergency use authorization to a COVID-19 vaccine as soon as this week. Schoch-Spana said more managing of public expectations needs to be done, however.
"I think there's a public expectation that the vaccine is coming and we're all going to get it. The reality is it's going to be coming slowly at first and in limited amounts," she said.
Balkus said the news around the vaccine is "remarkable and thrilling." It can often take years to get a safe and effective vaccine for a disease and is something some work their entire careers on, but now, "the biggest thing at this point is to stay vigilant."
"This is the time to go all in on protecting your family, protecting yourself, so you and your loved ones are able and still there to get the vaccine," she said.
Follow USA TODAY's Ryan Miller on Twitter @RyanW_Miller
This article originally appeared on USA TODAY: COVID-19 pandemic has changed since March: More deaths, vaccine closer

