It’s been 40 years since the first reported cases of AIDS. While treatments have come a long way, a vaccine remains elusive.

As New York's hospitals filled with pneumonia patients last spring, Dr. Michael Gottlieb flashed back to the earliest days of another mysterious illness.
For months, Gottlieb had vainly treated a young man with an unrelenting fever. The man developed pneumonia from a usually harmless virus and his mouth was covered with a fungus that made it hard for him to swallow or eat.
Another young man soon turned up with similar symptoms. Then, over the course of a few months, three more previously healthy Los Angeles men came down with the same constellation of problems.

As he watched them die, Gottlieb was both concerned and intrigued. At 33, he was roughly the same age. Their care became personal as well as professional.
Gottlieb and several colleagues contacted the Centers for Disease Control, which asked them to write up their findings. On June 5, 1981, exactly 40 years ago, their report was published, describing the cases of these five, young gay men whose immune systems had suddenly stopped protecting them, defying every treatment Gottlieb and others tried.
The condition didn't have a name then, but it would become known as AIDS, acquired immunodeficiency syndrome, and the report Gottlieb and his colleagues wrote would become the first official record of a disease that has since claimed more than 33 million lives around the world.
COVID-19 has done its work faster – infecting at least 172 million people and killing 3.7 million of them in less than 18 months.
But those who were around for the earliest days of AIDS say the parallels are unmistakable: a deadly pneumonia, a virus that seemed to target certain communities though none was immune, people unknowingly infecting loved ones, friends and strangers.
Like Gottlieb, many of the doctors and researchers whose career paths were defined by AIDS are now treating COVID-19 patients.
"You start from ground zero and then you build the plane as you're flying it," Gottlieb said of treating both diseases in their early days. "There was this sense of helplessness, of winging it, of doing the best you can with less than adequate tools and learning as you went."
The differences between the diseases are striking, too.
While COVID-19 was identified and brought to public attention within weeks, the first report of AIDS likely lagged years behind symptomatic cases, and diagnostic tests took five years to develop.
The human immunodeficiency virus that causes AIDS wasn't identified until 1983, two years after that first official record; researchers released the detailed genetic code of the SARS-CoV-2 virus in January 2020, less than a month after it came to global attention. With that code in hand, scientists immediately began developing highly effective COVID-19 vaccines, a triumph that still escapes HIV researchers.
"There's really an extraordinary difference in the pace of reaction to these pandemics," said Dr. Bruce Walker, a Harvard physician-scientist who has spent decades treating HIV–positive patients and working to better understand the disease.

The hopelessness and desperation of HIV/AIDS struck deep and hard, first among gay men, and then across the world's poorest communities, including in the United States.
With COVID-19, racial and socioeconomic disadvantages became quickly evident, with lower-income communities of color disproportionately affected. But it also spread far and fast, touching nearly every community on all seven continents.
Dr. Julie Gerberding was a young medical intern in San Francisco when the first AIDS patients began arriving: first one, then three, then 12. By the time she finished her intern year in June 1982, nearly all her patients had some manifestation of AIDS, and she often learned how to treat them by asking what they needed.
Later, as a federal official, she helped respond to the first SARS epidemic in 2002 and then, in 2009, while head of the CDC, she helped the country prepare for the H1N1 flu pandemic.
With COVID-19, she's seeing history repeat itself.
"We've watched a lot of the same issues play out over and over again," said Gerberding, now executive vice president and chief patient officer at Merck. She describes an "unwillingness to accept that something new and important has emerged and could get a whole lot worse."
Though both pandemics are far from over globally, in the United States, officials talk about ending HIV/AIDS within a decade with medications and prevention measures. Vaccines and public health efforts have cut COVID-19 infections here by more than 90% since January's peak.
"For those who are skeptical of science and we've heard a lot about that in COVID," Gottlieb said, "we might look to HIV as evidence that science does work."
Medications that protect, prevent
The greatest accomplishment of HIV science was the medications that turned the virus from a death sentence into a chronic, manageable disease.
The first one, azidothymidine or AZT, a repurposed cancer drug approved in 1987, was only slightly helpful. Side effects of AZT and other early drugs were considered worse than the disease, like being on chemotherapy every day for life.
Just a few years later, in 1989, Daria Hazuda joined the search for HIV/AIDS medications.
At one of her first scientific meetings, researchers presented the triple-combination drugs that would transform treatment. "People were astonished," Hazuda said. "I remember sitting in the audience thinking: 'I'd better find something else to work on. This has been solved.'"
But then, as she recalls it, a doctor stood up and told his colleagues: "Look at what we're asking our patients to do." People had to swallow a fistful of pills three times a day. They suffered horrible side effects. "Now that we know it's possible, let's go back and do it right," Hazuda remembers him saying.
That idea – that real people have to live every day with the drug therapies she developed – became a driving force in her career, Hazuda said. At drug company Merck, she went on to help create the drug Isentress, the first of a new class called integrase inhibitors, which were less toxic and easier for patients to manage.

Now vice president for infectious diseases at Merck, Hazuda hopes to keep improving the medications, working toward one pill a week instead of a day, or long-term injectables that would last three months or even a year.
It's still a challenge, she said to reach everyone who needs treatment or could be helped by taking the same drugs to prevent infection.
"It's fascinating to see how far we've come and how far we still need (to go)," Hazuda said.
For Bruce Richman, the revelation that would change his life came in 2012. He had been diagnosed with HIV in 2003, and though he took his medication faithfully – four pills a day – he considered himself a disease vector, toxic even.
"I had given up the concept of being intimate without fear," Richman said. "The idea that I could pass on HIV to somebody was just too much."

Nine years after his diagnosis, he was finally told that because he took his HIV medications reliably, his viral loads were undetectable. That meant he couldn't pass on HIV.
The finding so moved him that he's dedicated his life since to getting the message out: undetectable equals untransmittable, or "U=U."
Public health officials often avoided telling patients, worried it would make HIV-positive people think they didn't need their medications or make them vulnerable to other sexually transmitted diseases.
Richman, founding director of the Prevention Access Campaign, believes it's far more powerful to let people know they are not dangers to society, just as people vaccinated against COVID-19 are relieved to know they can no longer make others sick.
"With COVID, I think people are going to understand a little bit of what it's like to be afraid of passing on a virus to the people you love," he said. "People with HIV have lived with that fear for decades."
Moving toward the end
Walker already had spent years watching his patients waste away from AIDS when a healthy-looking man bounded into his office one day in 1994 asking how long he had left to live. The man had been infected 15 years earlier but had defied every expectation of his death sentence.

Walker realized the man's immune system somehow kept HIV in check without medication. That launched Walker on a decadeslong quest to understand people he calls "elite controllers," whose bodies seem to know how to control HIV.
In 2009, with a $100 million philanthropic donation, Walker founded the Ragon Institute of MGH, MIT and Harvard, an interdisciplinary scientific institute aimed at unraveling the mysteries of the immune system. One of its steering committee members is credited with developing Johnson & Johnson's COVID-19 vaccine.
Now, Walker, who continues to direct the institute, believes he understands how elite controllers contain and even eliminate the virus.
He and his colleagues have designed a vaccine with the idea of providing recipients the power of an elite controller.
"We don't have proof we can do that yet, but we have a really strong rationale for this," Walker said.
The vaccine will be based on the mRNA technology proven through COVID-19 vaccines, and will target areas of the virus that can't mutate. Walker hopes to begin testing it within a year.
Phill Wilson was 24 in 1981 when his swollen lymph nodes suggested he had been infected. His formal diagnosis didn't come until 1986, delayed by five years because of a lack of testing. His doctor said he had six months to live.
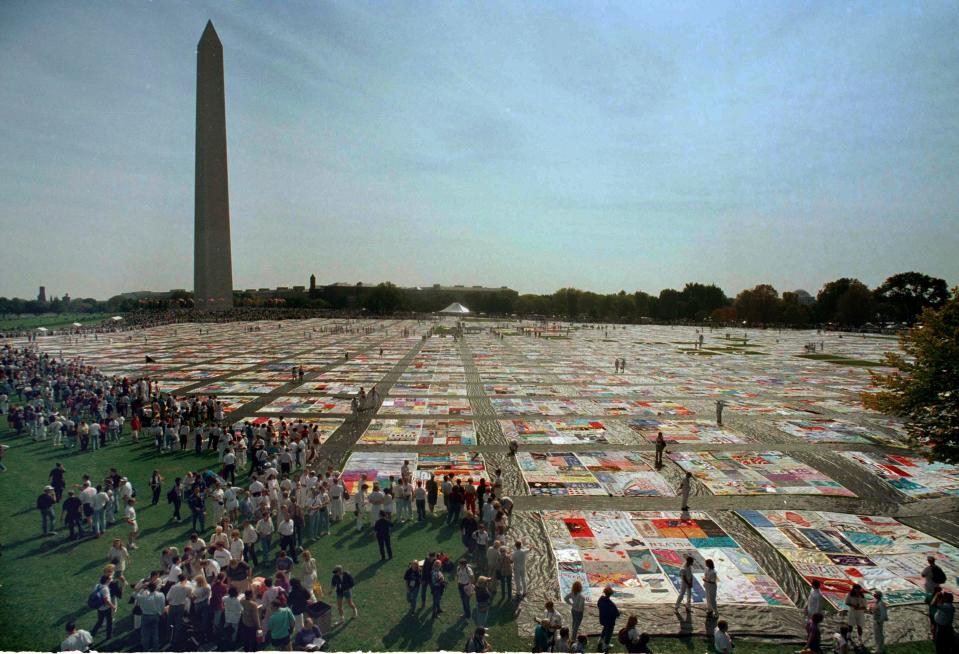
He kept an address book in those days before cellphones. Every time a friend died of AIDS, Wilson would put a checkmark next to that person's name. He lost the address book around 1987, he estimates. By then, he had added 220 checkmarks.
His own partner died in 1989. "While it was absolutely devastating to lose Chris, he was not the only loss that day (to AIDS)."
Wilson said he still hasn't completely come to terms with the grief.
"This went on from 1982 to 1997 – that's 15 years of that kind of intense dying," he said. "It was impossible to process it or to process any one death, no matter how close that death was to you."

In 1997, Wilson ended up in an intensive care unit in Los Angeles, connected to tubes and unable to speak. His mother flew in from Chicago expecting to watch him die. Instead, he got his first doses of protease inhibitors, the drugs that transformed the fight against HIV/AIDS.
"Dorothy landing in Oz and all of a sudden the world is in Technicolor … that's what protease inhibitors were like," Wilson said. He bounced back "like Lazarus."
He attributes his long-term survival with HIV to many factors including luck, a focus on living rather than dying, periodic medication vacations in the early days to avoid drug resistance, and his large extended family.
"I am alive today because I personify what happens when people with HIV/AIDS have the love and support we need and deserve from family and friends," he said.
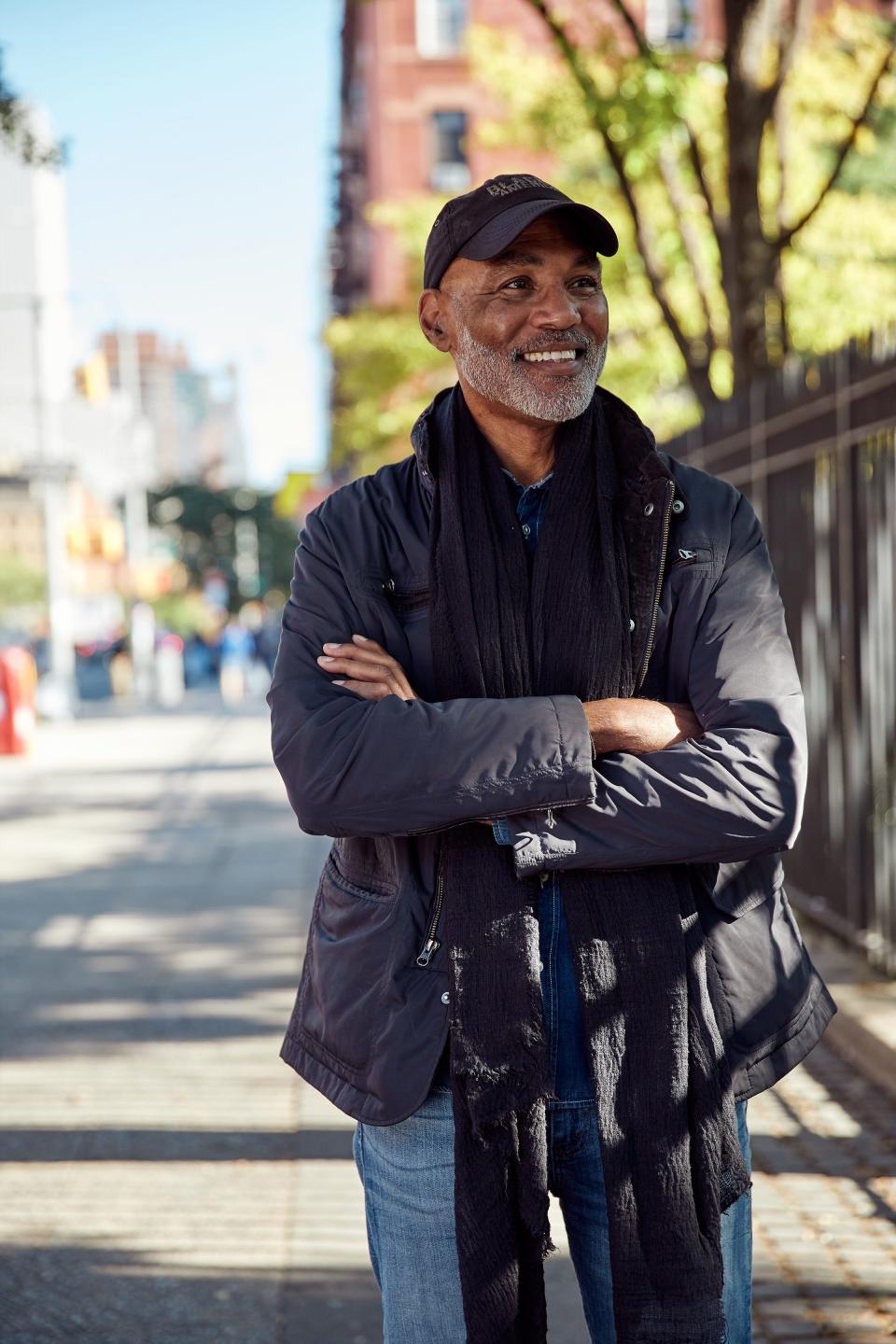
Early on, Wilson decided to become an activist and co-founded the Black AIDS Institute.
Raniyah Copeland is now the group's president and CEO, calling attention to the fact that both COVID-19 and HIV/AIDS have disproportionately affected people of color.

Over half of new HIV cases in the U.S. are in Southern states where many people have limited access to health care, Copeland said
"What we see is a widened disparity of HIV, which is part of what makes this 40-year-moment hit so hard," she said. "We've come so far, yet we're in the same place as we were 40 years ago when we look at who is being most impacted."
Aging with HIV
Wilson was an early adopter of medications, trying nearly every new HIV drug as it came on the market. He doesn't even remember how many pills he had to pop every day at the height, but thinks it was somewhere between 10 and 15, each of which had its own requirement for before a meal or after, "all sorts of crazy regimens."
Now, he said, he takes nearly as many medications, but only one is to keep his HIV under control. The rest, he said, are because he's a 65-year-old man: "I have lived far past my expiration date."
Aging with HIV has become a key focus of another activist, Jayson Duley, 56, who has been HIV-positive for 20 years.

Duley, director of global security for a software company, said his view of HIV/AIDS has changed with the decades.
As a young man, discovering his sexuality, he saw AIDS as a death sentence. His own diagnosis came after treatments had turned it into a chronic infection, and he has lived through a number of improvements in those medications.
Envisioning the next 20 years, he's hoping treatments will continue to improve, offering longer-term protection. Maybe vaccines will even provide a cure.
But in the meantime, data suggests HIV-positive people age faster than normal, developing high cholesterol and blood pressure and heart issues at younger ages, though it's still unclear whether that's from the virus or the medication.
"Aging with HIV is scary," Duley said. "Aging with HIV is our next challenge."
For his part, Michael Gottlieb, now at APLA Health in Los Angeles, said he's satisfied with the trajectory of his career. He has been caring for patients for more than 40 years.
In 2020, he began treating HIV-positive patients with COVID-19, who all fared well. "I've been able to save some lives," he said. "That's been the most satisfying thing."
Contact Karen Weintraub at kweintraub@usatoday.com.
Health and patient safety coverage at USA TODAY is made possible in part by a grant from the Masimo Foundation for Ethics, Innovation and Competition in Healthcare. The Masimo Foundation does not provide editorial input.
Timeline of key moments

June 5, 1981: First official description of the illness that would become known as HIV/AIDS.
Sept. 24 1982: The mysterious ailment was named acquired immunodeficiency syndrome, or AIDS by the Centers for Disease Control.
May 20, 1983: French researchers announce the discovery of the virus that causes AIDS and name it human immunodeficiency virus or HIV.
December 1984: Ryan White, a 13-year-old from Indiana, is diagnosed with HIV/AIDS after a blood transfusion. White died in April 1990, just before he would have graduated from high school. The Ryan White Comprehensive AIDS Resources Emergency (CARE) Act, passed in August 1990, provides health care for HIV-positive people who cannot afford their medications.
Oct. 2, 1985: Actor Rock Hudson died of AIDS and his friend the actress Elizabeth Taylor became an AIDS advocate
March 1987: The cancer drug azidothymidine or AZT was approved for use in AIDS patients. It offered only marginal benefit over placebos, said Dr. Michael Gottlieb, who was involved in a clinical trial, but it was proof that a drug could act against the virus.
Nov. 7, 1991: Magic Johnson announces his retirement from basketball after his diagnosis with HIV. He goes on to raise awareness and more than $10 million to support people with HIV/AIDS.
December 1995: The first of a new class of drugs called protease inhibitors, called saquinavir, was approved. Combined with AZT and a similar drug, these drug "cocktails" began to lower the viral load of people with HIV to undetectable levels, though the regimen was difficult to follow.
Nov. 15, 2007: Raltegravir (Isentress), the first drug of a class called integrase inhibitors was approved and became a component of combination therapy.
July 16, 2012: The drug Truvada was approved for pre-exposure prophylaxis, or PrEP, in which healthy people take antiretroviral drugs to reduce their risk of catching HIV.
This article originally appeared on USA TODAY: First AIDS cases 40 years ago: Treatments far better, still no vaccine

