Diabetes Insipidus: Another Chronic, But Different, Type of Diabetes
Medically reviewed by Danielle Weiss, MDMedically reviewed by Danielle Weiss, MD
Diabetes insipidus (DI) is a rare disorder in which the body cannot properly regulate fluids. It is not related to the more common diabetes mellitus, in which the body cannot properly regulate blood glucose (sugar) levels. People with DI have a higher-than-usual urine output.
This article will explore the symptoms of diabetes insipidus, its causes, risk factors, and treatment.
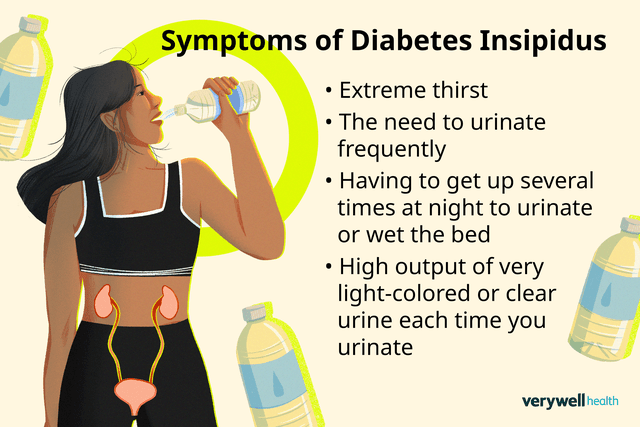
Illustration by Julie Bang for Verywell Health
Are My Symptoms Diabetes Insipidus or Regular Dehydration?
While one of the hallmark symptoms of diabetes insipidus is thirst, there is more to it than what you would experience with regular dehydration. Most healthy people produce around 1 to 3 quarts (32–96 ounces) of urine a day. However, people with DI may produce up to 20 quarts (640 ounces) of urine in a day.
Distinguishing Symptoms
The main symptoms of diabetes insipidus are:
Having to get up several times at night to urinate or wet the bed
High output of very light-colored or clear urine each time you urinate
The main complication of DI is dehydration (the body does not have enough fluids due to high fluid output and/or insufficient fluid intake); dehydration can lead to electrolyte imbalances. Electrolytes are charged minerals in the blood, such as sodium, potassium, and calcium.
Symptoms of dehydration include:
Dizziness
Light-headedness
Dry skin
Crying without tears (infants and young children)
No wet diapers for three hours or more (infants and young children)
When to Ask a Provider
If you are not already diagnosed with diabetes insipidus and are experiencing any symptoms of DI or dehydration, contact a healthcare provider for further evaluation. They can review your health and medical history, perform a physical examination, and order certain urine and blood tests to help check for DI.
Severe dehydration should be treated promptly. It can lead to serious complications such as seizures, irreversible brain damage, and even death. Seek medical attention immediately if you feel any of the following:
Confusion
Dizziness
Sluggishness
Subtypes of Diabetes Insipidus
Though the exact cause may vary, diabetes insipidus is usually due to problems with a hormone called vasopressin, also called antidiuretic hormone (ADH). Vasopressin helps the kidneys regulate the amount of fluid in the body.
The four main types of DI are classified depending on the specific cause of vasopressin dysregulation. They include:
Central diabetes insipidus (also called arginine vasopressin deficiency) is when the body doesn’t make enough vasopressin.
Nephrogenic diabetes insipidus is when the kidneys don’t respond to vasopressin as they should.
Dipsogenic diabetes insipidus is when there is a problem with the hypothalamus (a hormone-producing area of the brain that makes vasopressin), causing you to feel thirsty and drink more fluids.
Gestational diabetes insipidus is when a pregnant person’s placenta makes too much of an enzyme that breaks down vasopressin in the body during pregnancy.
Who Gets Diabetes Insipidus?
People of any age can develop diabetes insipidus. Risk factors include:
Having family members with diabetes insipidus
History of a major head injury or brain surgery
Taking medications that can cause kidney problems, such as some bipolar disorder medicines and diuretics (water pills)
Having a metabolic disorder, such as low blood potassium or high blood calcium levels
How Much Water to Drink With Diabetes Insipidus
Staying hydrated is important when you live with diabetes insipidus. Drinking enough water and other liquids to prevent dehydration is the main treatment for diabetes insipidus.
No set amount of water to drink per day has been established for people with diabetes insipidus. Thirst levels can vary depending on the severity of the condition, as well as the specific type of DI you have.
Monitoring your urine color (aiming for pale yellow or straw-colored urine) can help you determine if you need to drink more water. Talk with your healthcare provider to determine how much water you need to drink each day for DI.
Diabetes Insipidus Treatment
Aside from drinking enough water, treatment options depend on the type of DI. Specialists who help treat DI include endocrinologists (specialists in hormonal conditions) or nephrologists (specialists in kidney conditions). Treatment may include:
Hormone replacement therapy: Ddavp (desmopressin), an artificial form of vasopressin, may be recommended for central diabetes insipidus and gestational DI.
For nephrogenic diabetes insipidus: If caused by a medication, discontinuing that medication may resolve the condition. Diuretic medications, such as thiazide, help decrease the amount of urine the kidneys produce, and nonsteroidal anti-inflammatory drugs (NSAIDs), such as Advil or Motrin (ibuprofen) or Aleve (naproxen sodium), may also be recommended. Thiazide diuretics may increase urine production in other conditions, but they reduce it in this condition.
Managing Effects of Chronic Diabetes Insipidus
Some of the chronic effects of DI, such as excessive thirst and frequent urination, can impact daily life. Getting into the habit of drinking more water and having a water bottle with you at all times can help you stay hydrated.
Sucking on ice chips or sugar-free candies can help keep your mouth moist and increase saliva. If you are waking multiple times at night to urinate, a healthcare provider may recommend taking a small dose of desmopressin before going to bed.
Maintaining proper nutritional intake is also important to prevent unintentional weight loss, lower-than-expected growth (in children), or nutrient deficiencies.
Though DI can be a chronic condition, with proper treatment, people with DI can expect to live a full and normal life.
Summary
Diabetes insipidus is a rare disorder in which the body cannot properly regulate fluids, usually caused by dysregulation of a hormone called vasopressin. DI is not related to the more common diabetes melitus, in which the body does not properly regulate blood glucose (sugar) levels.
There are four main types of DI, depending on the cause of the vasopressin dysregulation. Hallmark symptoms of DI include the need to urinate frequently, excessive thirst, and having a large output of clear or light-colored urine.
DI can lead to symptoms of dehydration, such as dry mouth, dry skin, dizziness, light-headedness, fatigue, or dark-colored urine.
The main treatment for DI is drinking enough water to prevent dehydration. Other treatments will vary depending on the type of DI you have but may include medications and stopping medications that can trigger DI.
Read the original article on Verywell Health.

